‘I survived the unsurvivable’: Mother of 2 suffers massive heart attack after feeling subtle symptoms more common in women

On a Tuesday morning in July 2022, Sarah Casalan Bittle awoke with what she thought was indigestion from a hamburger she’d eaten the night before. The busy single mother of two from suburban Northbrook brushed it off and went about her week. Her mother was visiting, and she was still riding high from a conference the previous week where she’d shared a stage with the CEO of her company.
The next night, Casalan Bittle tucked her children in to bed and went to sleep. She awoke in the middle of the night with nausea and sat on the bathroom floor. She waited to be sick, but never vomited. Then she had trouble standing.
“The lizard part of my brain started yelling: ‘Something’s wrong. Get up! Get up off the floor,’” Casalan Bittle said. “I stood up, and that’s when I first felt the chest pain.”
Casalan Bittle made it to her mother’s room and said, “I don’t know, but I think I’m having a heart attack.” She was unconscious five minutes later.
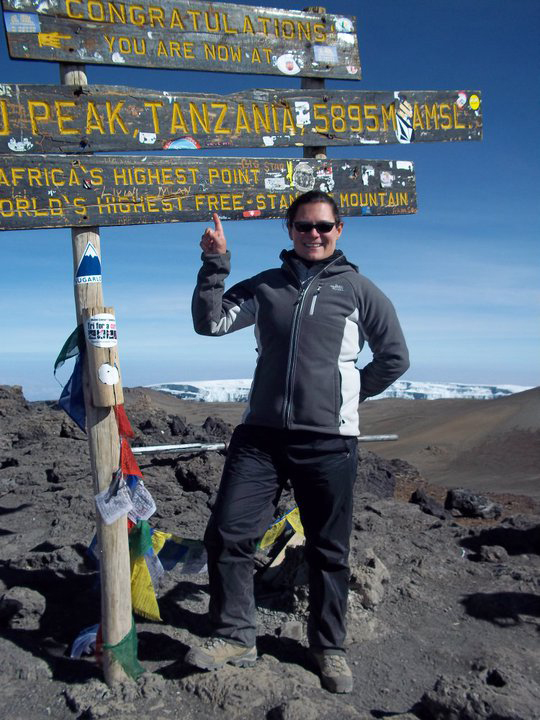
An active woman who traveled the world and once climbed Mount Kilimanjaro, Casalan Bittle, then 47, had suffered what’s commonly known as a widowmaker heart attack. Her left anterior descending (LAD) artery was 100% blocked. She estimates she was having a heart attack for about 90 minutes before she realized what was happening. After all, her physical three months earlier showed no risk factors for cardiovascular disease.
“Why would I ever think I was having a heart attack?” she said.
The heart attack was only the beginning of a journey that came with harrowing setbacks but ultimately led to recovery.
"Touch and Go"
Casalan Bittle’s symptoms were normal signs of a heart attack in women.
The symptoms women experience when they have a heart attack are often different from men. Signs can be subtle for men and women, but the ‘Hollywood heart attack’ — clutching the chest and falling to the ground — is what we see more in men. For women, a heart attack may look nothing like that.
Casalan Bittle was rushed to a nearby hospital, where she went into cardiac arrest twice in the cardiac catheterization lab while her blocked LAD artery was repaired. She received a heart pump to assist with blood flow and was ultimately put on ECMO, a form of life support and the highest level of cardiac support a patient can receive aside from major surgery. At that point, doctors told Casalan Bittle’s family her best chance for survival was a transfer to UChicago Medicine to be evaluated for an emergency heart transplant.
Smith was Casalan Bittle’s admitting physician when she arrived at the Hyde Park academic medical center. He was concerned her heart wouldn’t recover after coming off ECMO and she would need a transplant to survive.
In the meantime, Casalan Bittle awoke for the first time and saw a white board that said “Saturday.” She’d been unconscious about 60 hours. Her first thought was of her children. Then she saw her sisters, who had flown in from the East Coast. That’s when she realized how serious her situation was.
Smith said it was “touch and go,” but after coming off ECMO and certain medications, Casalan Bittle’s heart recovered enough to avoid a transplant. Smith and UChicago Medicine cardiologist Bow (Ben) Chung, MD, who cared for Casalan Bittle throughout the week, praised the level of support she had received before her transfer to UChicago Medicine.
“It proved to be enough where we were able to get her to some degree of heart recovery over the course of the week,” Chung said.
Casalan Bittle still faced challenges. A critical point came when her heart pump was removed and a clot formed in her femoral artery in her leg. She faced the loss of her foot as the clot cut off blood to her extremity. Casalan Bittle benefitted from the timely multidisciplinary care of the UChicago Medicine heart and vascular team.
“Her leg was at significant risk, but we were able to remove the blood clot in her right groin and do a direct repair on the right and left femoral arteries to restore the blood supply,” said UChicago Medicine vascular surgeon Ross Milner, MD, Section Chief of Vascular Surgery and Endovascular Therapy.
“Sarah’s case showcases how well we work together as a team,” Smith said. “If everything is done perfectly and patients are managed quickly from a team approach, they can do well overall.”
Casalan Bittle spent nearly two weeks in the hospital, followed by six weeks of outpatient therapy at Shirley Ryan AbilityLab where she worked to regain her strength. She wore a LifeVest — a wearable defibrillator — for three months and was put on a medication regimen for heart failure. Casalan Bittle went back to work and caring for her young sons, aged 8 and 7.
“My kids were all I really thought of when I was conscious,” she said. “I’m extremely grateful for my team at UChicago Medicine.”
A Daunting Setback
Casalan Bittle eased back into traveling for work, began a cardiac rehabilitation program, and started managing her heart failure with UChicago Medicine cardiologist Nitasha Sarswat, MD.
In February 2023, Casalan Bittle began experiencing a “tickle” sensation in her chest. She went to the emergency room after a difficult cardiac rehab session, but providers couldn’t find anything wrong. The next week at a routine appointment, Sarswat ordered a stress test. The results were concerning enough to send Casalan Bittle back to the cardiac catheterization lab.
She received upsetting news. Doctors discovered a 70% blockage in her left main coronary artery, which meant Casalan Bittle would need bypass surgery. After everything she’d been through, the thought of open-heart surgery felt overwhelming.
“I always anticipated setbacks along the way, but I wasn’t expecting this,” she said. “I pretty much told everybody to kick rocks.”
But Casalan Bittle was a candidate for a totally endoscopic coronary artery bypass (TECAB) surgery, a unique type of robotic heart surgery commonly offered at UChicago Medicine. The minimally invasive, closed-chest procedure would spare her from having her breastbone split and going on a heart-lung bypass machine. She would have a shorter hospital stay and a quicker recovery.
Cardiac surgeon Husam H. Balkhy, MD, performed Casalan Bittle’s TECAB surgery on March 3. She was home two days later.
Balkhy, Director of UChicago Medicine’s Robotic and Minimally Invasive Cardiac Surgery Program, has performed over 2,000 robotic heart surgeries in his career and said that although a few centers offer robotic surgery for valves, UChicago Medicine is the only center in the U.S. to offer totally endoscopic robotic surgery in the coronary sphere.
“Not only is Dr. Balkhy an expert and pioneer in his field, but he’s also a leader who has built an extraordinary team that’s centered around patient care,” Casalan Bittle said. “People were asking if I was scared or nervous. Not in the slightest. Not even a little tiny bit.”
"The most blessed year of my life"
What led to Casalan Bittle’s heart attack and subsequent blockage remains unclear. But Chung said that her story can still serve as a reminder for women to be aware that heart attack symptoms they experience may be different from men’s.
“If you have unexplained chest discomfort that won’t go away, it’s best to go to urgent care or an emergency department,” Chung said. “Be aware of abdominal pain or pain in your neck, jaw, shoulders or arm. Other symptoms can be shortness of breath, nausea, vomiting or heavy sweating. If you know why these symptoms are happening, it’s less likely you’re having a heart attack. The concern is when you can’t explain why you feel unwell.”
“Sarah’s symptoms were very subtle,” Smith said. “It really drives home the point of how different symptoms can be in men and women. Data show us that women often come to the hospital later than men, and their heart attacks are diagnosed later, which means they’re more likely to have worse outcomes because of that delay.”
Today, Casalan Bittle is listening to her body, resting more and accepting that she’s not yet 100%. She’s not sure she wants to return to her pre-heart attack lifestyle and the amount of stress she lived with every day. For now, she’s focused on healing and her family.
“I have every reason to say this last year was the worst year of my life, but I don’t,” Casalan Bittle said. “It was the most blessed year of my life. The most positive year of my life. I survived the unsurvivable, right? I have access to extraordinary medical and rehabilitative care. That’s a privilege, and I’m so extremely lucky. And now I’m going to go live a long life.”

Heart Failure and Transplantation
At the University of Chicago Medicine, we bring the best minds in medicine together to meet the needs of patients facing heart failure and transplant.
Read more about our heart failure expertise
Women's Heart Disease Program
Our Women's Heart Disease Program offers a full scope of cardiovascular care for women. At UChicago Medicine, we focus on understanding the unique causes of heart disease in women and providing treatment to prevent or slow the progression of heart disease.
Read more about heart disease in women