Synthetic Midurethral Sling
Midurethral slings are the most common and best researched procedures for stress urinary incontinence. They are safe, effective and can improve quality of life for many women. In addition to having high cure rates, midurethral slings also have fast recovery times, allowing women to resume their active lifestyle within days.
How is the procedure performed?
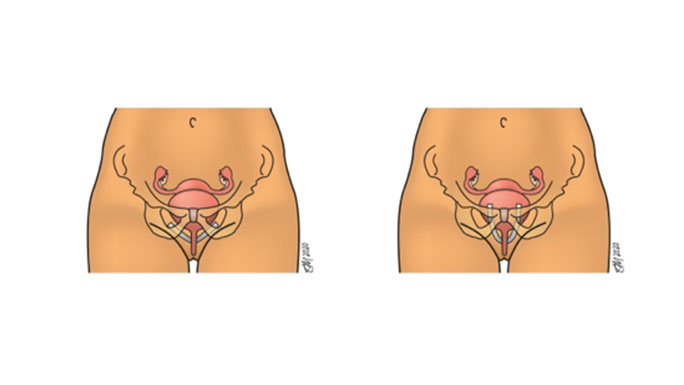
During this procedure, a permanent synthetic mesh made of polypropylene (soft plastic material) is placed under the urethra through a small incision in the front of the vaginal wall while the patient is under sedation (“twilight”) anesthesia. The sling supports the urethra during increases in abdominal pressure and prevents urine leakage. There are different approaches for midurethral slings including retropubic and transobturator approaches. In the retropubic approach, the sling passes behind the pubic bone, whereas in the transobturator approach the sling exits where the thigh meets the groin.
How successful is the sling procedure?
Synthetic retropubic midurethral slings have extraordinarily high success rates. Numerous high quality national and international studies have demonstrated efficacy greater than 90%. Retropubic and transobturator slings have similarly high success rates, although long-term studies favor the success of the retropubic approach.
What are the risks of a sling procedure?
The synthetic retropubic midurethral sling has been extensively researched. The Food and Drug Administration (FDA) supports the safety and effectiveness of midurethral slings, which have largely replaced older, more traditional procedures for stress urinary incontinence. Urinary tract infections are the most common side effect following synthetic midurethral slings. Both retropubic and transobturator slings have a small risk of a mesh exposure (a small portion of the mesh can peak through an area in the vagina). This side effect is easily managed with either non-surgical or surgical treatment.
What does recovery look like?
Owing to the minimally invasive approaches used by your University of Chicago Medicine urogynecologic surgeon, you will be able to go home the same day as surgery. Most women feel back to normal within two weeks following surgery.
Enhanced Recovery After Surgery (ERAS) Program
To help you properly heal and get back to do the activities you love, our urogynecologists have developed an Enhanced Recovery After Surgery (ERAS) Program to reduce post-operative pain, nausea and fatigue. As quality-of-life surgeons, we are passionate about restoring your quality of life, and aim to return you to the activities that you find interest in as quickly as safely possible. We allow you to resume activity as you see fit, listening to your body and its response to physical activity. However, we do ask you to refrain from sexual activity for several weeks while the stitches in your vagina heal. Most women feel back to normal within two to four weeks following surgery.
Meet Our Urogynecologists

Urogynecology and Reconstructive Pelvic Surgery

Urogynecology and Reconstructive Pelvic Surgery

Urogynecology and Reconstructive Pelvic Surgery

Urogynecology and Reconstructive Pelvic Surgery

Urogynecology and Reconstructive Pelvic Surgery
