Anal (Fecal) Incontinence
What is Anal Incontinence?
Anal incontinence is the accidental loss of bowel control that results in the leakage of gas (flatal incontinence) or stool (fecal incontinence). Anal incontinence is common, affecting 10 percent of women. But because the condition can be embarrassing to talk about, many are reluctant to seek care. Anal incontinence often occurs with other pelvic floor disorders, including urinary incontinence. In fact, up to 20 percent of women who have urinary incontinence also suffer from fecal incontinence.Symptoms of Anal Incontinence
Signs of anal incontinence include:- Stool leakage
- Inability to control passage of gas
- Urgency to have a bowel movement
Causes of Anal Incontinence
The anal sphincter and pelvic floor muscles help control your bowel movements and flatus (passage of gas). Anal incontinence occurs when there is damage to the muscles and/or nerves in these important structures, so they do not function normally.
Sometimes there is damage to the anal sphincter muscle during childbirth, which is identified and repaired at the time of delivery. Most often, symptoms of anal incontinence don’t develop until later in life. Although the most common risk factors for women are childbirth and aging, other risk factors for anal sphincter and pelvic floor muscle injury include:
- Inflammatory bowel diseases (such as ulcerative colitis or Crohn’s disease)
- Chronic diarrhea
- Previous surgery on the colon or anus
- Pelvic radiation therapy for cancer
- Rectal prolapse
- Perineal tears during childbirth
What to Expect During Your Evaluation for Anal Incontinence
At your first visit, your urogynecologist will ask you specific questions such as:
- How often do you experience anal incontinence?
- In what situations do you typically experience bowel leakage or pass gas accidentally?
- Do certain foods make your symptoms worse?
- What is the consistency of your bowel movements?
Keeping a diary of your bowel symptoms and habits may help you answer these questions.
A physical exam is also an important step in the evaluation and can identify conditions like rectal or vaginal prolapse, pelvic floor muscle dysfunction or hemorrhoids that may be related to your symptoms. During your physical exam, your urogynecologist will evaluate your pelvic floor muscles, anal sphincter and pelvic organ supportive tissues.
Tests to Diagnose Anal Incontinence
Many times, additional testing can help your care team identify issues with your pelvic floor muscles and anal sphincter that may cause your symptoms. Your urogynecologist may recommend tests that include:
- Pelvic floor (endoanal) ultrasound to understand potential causes affecting your anal sphincter and pelvic floor muscles
- Anal manometry to learn more about your sensation and the pressures in your anal canal
- MRI defecography to examine the positions of your pelvic organs when you have a bowel movement
We will also make sure that you have been screened for colorectal cancer especially if you have a change in your bowel symptoms, particularly blood in the stool.
Treatments for Anal Incontinence
Based on your evaluation and test results, your urogynecologist can discuss a range of options, from dietary changes to minimally invasive surgical procedures, for the treatment of anal incontinence. Your urogynecologist will work with you to determine the best approach to meet your goals.
Lifestyle and Dietary Changes
Lifestyle and dietary changes can ease symptoms of anal incontinence by improving the consistency of your stool. These changes include:
- Adding more soluble fiber to your diet. Most women will need to take a psyllium-based fiber supplement to achieve the correct stool consistency. This particular kind of fiber works to add “bulk” to the stool to make it easier for your rectum to control.
- Avoiding substances that can cause loose stools like artificial sweeteners, alcohol and caffeine.
Your urogynecologist may recommend trying lifestyle and dietary changes first or in combination with other treatments like pelvic floor therapy, which can provide effective symptom relief for most women.
Medication
Medications like loperamide (Imodium) can improve anal sphincter tone and/or slow the passage of food through the colon.
Pelvic Floor Physical Therapy
Pelvic floor physical therapy can teach you how to improve your anal sphincter and pelvic floor muscle function to manage anal incontinence. Your pelvic floor physical therapist may use biofeedback, a technique that helps you become more aware of your body’s functions so you can control them. In urology and gynecology, biofeedback is typically used to help patients locate and strengthen their pelvic floor muscles.
Procedures for Anal Incontinence Treatment
For those who still have symptoms after trying lifestyle changes, medication and/or physical therapy, other procedures for anal incontinence include:
Sacral neuromodulation is a minimally invasive procedure that effectively treats anal incontinence (as well as urgency urinary incontinence) by providing gentle stimulation to the nerves that control the bladder and bowel.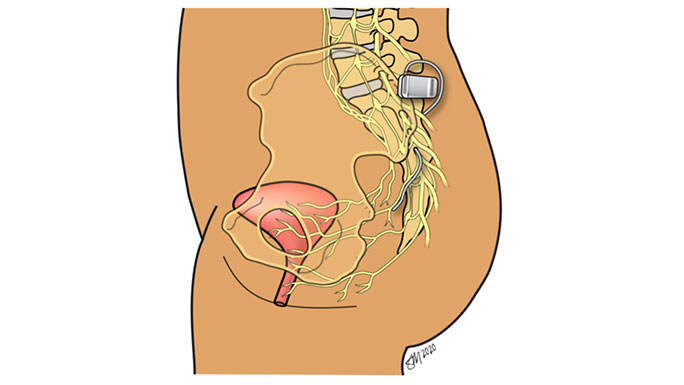
If you have a tear in your anal sphincter (such as from a birth injury or a fistula) and other treatments have failed, you may be a candidate for a minimally invasive, same-day surgical procedure called anal sphincteroplasty. During a sphincteroplasty, a surgeon repairs the torn anal sphincter muscle and reconstructs the perineal body (the muscles separating the vagina from the rectum). This does not involve any incisions on the abdomen. Typically, women will have pelvic floor physical therapy after surgery to help the newly reconstructed pelvic floor and anal sphincter muscles function properly.
Meet Our Urogynecologists

Urogynecology and Reconstructive Pelvic Surgery

Urogynecology and Reconstructive Pelvic Surgery

Urogynecology and Reconstructive Pelvic Surgery

Urogynecology and Reconstructive Pelvic Surgery

Urogynecology and Reconstructive Pelvic Surgery
