Head and Neck Cancer Treatment

At UChicago Medicine, our head and neck cancer team strives to provide effective treatment that gives the patient the best outcome, while preserving as much speech, voice and swallowing function as possible.
The earlier the cancer is diagnosed, the more likely the treatment will be successful. Matching the appropriate therapy to each patient is vitally important in all cancer care.
For head and neck cancer, treatment may involve a combination of surgery, radiation therapy and/or chemotherapy. Experts in surgery, medical oncology, radiation oncology, radiology and pathology meet regularly in a head and neck tumor board conference to carefully review cases and work together to develop the best care plan for each patient.
Head and neck cancer treatment options are determined by the stage of the cancer, the location of the tumor and other factors.
Treatments include:
UChicago Medicine physicians pioneered an innovative first-line combination chemotherapy and radiation therapy approach that effectively shrinks some head and neck tumors, reducing the need for surgery. Patients with any type of head and neck cancer may be candidates for this approach.
For many patients with head and neck cancer, surgery is the best option for a successful outcome. Our expert head and neck cancer surgeons work with radiation and medical oncologists to develop a tailored treatment plan.
No matter the type or stage of cancer, if surgery is required, our experts provide the most effective treatment to preserve as much breathing, eating, speech and swallowing function as possible.
Some procedures may be performed using minimally invasive techniques or robotic surgery, resulting in a quicker recovery and less pain and scarring than open procedures.
We perform the full range of minimally invasive and traditional surgical procedures to treat cancers of the head and neck, including:
Endoscopic surgery: A minimally invasive approach that uses thin instruments to remove tumors with pinpoint precision.
Transoral robotic surgery (TORS):Uses sophisticated robotic technology to remove hard-to-reach tumors through the mouth, rather than creating larger incisions in the neck or jaw. Learn more about transoral robotic surgery.
Transoral laser microsurgery (TLM): A minimally invasive treatment for cancer in the voice box. During TLM, the surgeon gets a magnified view of the tumor with a microscope, and then uses a laser to remove it with precision, limiting the damage to nearby healthy tissue. This procedure preserves tissue and structures critical to voice and swallowing function.
Our radiation oncologists use sophisticated methods to deliver precise treatments to tumors while sparing healthy tissue.
UChicago Medicine was one of the first hospitals in the nation to offer intensity modulated radiation therapy (IMRT) for head and neck cancer. With IMRT, the radiation beam is accurately shaped to follow the contours of the tumor and to avoid critical structures such as the salivary glands or the optic nerve.
Our team also uses image-guided radiation therapy (IGRT) to confirm the exact tumor position and make any needed adjustments before treatment begins. Experts at UChicago Medicine refined a 3-D imaging system for IGRT, resulting in improved treatment planning and quicker radiation therapy sessions for the patient.
In recent years, cases of head and neck cancer linked to the human papillomavirus (HPV) have increased dramatically. HPV is the most common sexually transmitted disease in the United States and is the cause of most cases of oropharynx cancer (cancer of the tonsils and base of the tongue). Risk factors and prognosis for HPV-associated tumors are different from other types of head and neck cancers.
Our team has extensive experience treating patients with HPV-positive head and neck cancer. And we are at the forefront of research into how HPV-associated cancers respond to treatments. Our goal is to tailor effective therapies to reduce side effects and improve overall quality of life. Examples of outstanding care include robotic surgery, making treatment less intense and therefore better tolerated, and using new approaches that harness the power of the immune system to fight HPV-associated cancer.
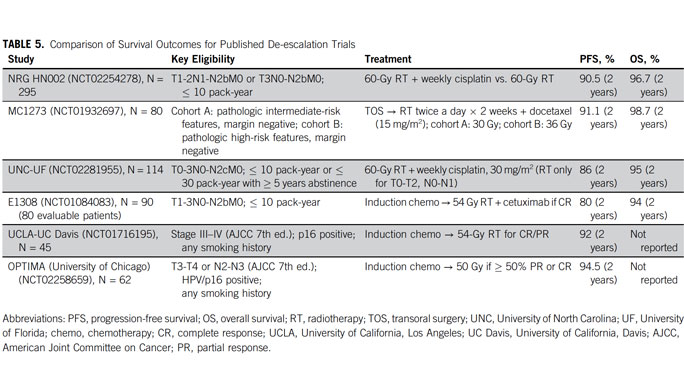
Read a Q&A about the role of HPV in head and neck cancer and how UChicago Medicine specialists are tailoring treatment for people with HPV-associated head and neck cancer. Our de-escalation approach resulted in the nation's leading survival rates: ~95% of patients were still alive after two years and patients treated with less radiation were less likely to need feeding tubes.
Immunotherapy — treatments that harness the power of the immune system to recognize and attack cancer cells — is an emerging treatment approach for head and neck cancer. Our physicians offer these treatments, in some cases as part of a clinical trial. As an example, a 2015 study here found that the anti-PD-1 immunotherapy pembrolizumab was effective in very advanced recurrent/metastatic head and neck cancers and roughly twice as effective as the best currently approved targeted therapy. In this study, immunotherapy was active across a wide range of patients, including HPV-associated and HPV-negative tumors.
Our head and neck cancer surgical team — which includes plastic and reconstructive surgeons who work with head and neck surgeons — are skilled at using organ-sparing and reconstructive techniques to maintain a patient’s physical appearance and function during and after treatment.
Patients with recurrent head and neck cancers often come to us after being told "nothing can be done." Our team believes that there is always something that can be done to support patients. Options may include surgery, radiation and/or experimental therapies. We work to provide pain relief, wound rehabilitation and hope for survival.
We are also leaders in re-irradiation — a second treatment, when necessary, of full-dose radiotherapy. This may involve a combination of radiation with chemotherapy and molecularly targeted agents.
Head & Neck Cancer: Q & A
Medical oncologist Alexander T. Pearson, MD, PhD, and nurse navigator Patricia Heinlen, BSN, RN, discuss head and neck cancer, including the HPV vaccine and how new treatment approaches are tailored to each patient's cancer type, making treatments more effective while reducing side effects.
And welcome to At The Forefront Live. Over the next half hour, we'll take your questions live. So start typing in the comments section, and we'll get to as many as possible. We will remind everyone that today's broadcast is not designed to take the place of consultation with your doctor. Now joining me today is physician Alexander Pearson and nurse navigator Patricia Heinlen. Welcome to the program.
Thank you.
Thanks.
First of all, there are a lot of unique head and neck cancer diagnosis. And what are the most common?
Yeah, thanks for asking.
Sure.
So the most common type of head and neck cancer, the one we see most frequently in our clinic, is called head neck squamous cell carcinoma, which encompasses the vast majority of different diagnoses. And there are two major subtypes that you may have heard about in the media and that's HPV positive and HPV negative. HPV means human papilloma virus, so virus related and virus unrelated cancers.
And interestingly, we hear a lot about HPV in the news recently, especially. And I think there are a lot of reasons for that. One involves the vaccine that people are being encouraged to have for their children or their teenagers. It looks like we're actually seeing a vaccination, or is it maybe the same vaccination is available for people older, is that correct?
Yeah, that's right. And you should talk to your doctor about the vaccination and if that's available to you. But the-- I think we're excited about this. Being cancer doctors, were excited about this. We certainly seen the trends for human papilloma virus related cancers related to cervical cancer start to change as more and more women are getting the HPV vaccine. So we hope that the same sort of trend will carry forward with head and neck cancers although the reality is that those changes, the decreases in cancer diagnosis rates, it's going to take decades before that manifests itself with an actual cancer clinics.
Explain this to me because I'm kind of curious about the APV, H-- excuse me-- HPV vaccination. Generally, we'd heard about it for younger folks. And now it looks like up to 45 is the cut off. And if you're over 45 at that point, no?
You know, it may be in the future that the criteria for diagnosis expands additionally best where it is now. This is-- we've-- this is the-- your insurance will cover it up to age 45 potentially depending on after a conversation with your doctor. And so I think it's just in terms of-- it may be that the benefit of the vaccination extends for older individuals. We don't know that yet. But the-- really, when this human papilloma virus affects the cells in your mouth or in your throat, it then takes additional potentially decades for those cells to become cancer cells. So it may be the--
If they become cancer cells at all.
If they become cancer cells at all, exactly. So it may be that for the oldest individuals, they can't derive the benefit over that decades long period to prevent any transition to cancer cells.
Excellent.
And Tricia, you mentioned that it takes a while. And talk to us a little bit about that if you will, please, just as far as the value of this and your opinion for patients potentially.
Well, like Dr. Pearson said, not every HPV cell will transform into cancer. So that's important to remember. And when you're thinking about the vaccines, we need to remember that it's not something that's going to turn something off immediately. And it's also not going to-- things are going to change into cancer immediately. So we have to think about that. And I think that's why the vaccine is only approved right now up to 45.
Sure. Whenever we talk about cancer, obviously people are afraid of cancer. And many believe it's a death sentence. But that's not true at all. In fact, we have this story of one patient who had throat cancer, got treatment, and is now living a very productive life.
[INAUDIBLE]
No, she's going to [INAUDIBLE] we're going to square up right underneath, and it will become super symmetrical at that point.
What time is it?
[INAUDIBLE]
We got an hour and a half.
I don't have my [INAUDIBLE].
About six years ago, I was diagnosed with stage four neck and throat cancer. So it was a shock to me. Of course, it was a huge, huge shock. You know, you're just into your 50s. You still feel a bit indestructible.
You're not thinking that cancer is going to be part of your life. Come over here for a second. Look right here, my hand.
[INAUDIBLE] this camera.
Well, you can get behind me.
It was very scary. Very difficult for me. We went up to our cabin in Michigan, and he actually made dinner and everything and just we started talking about just a lot of different things. And all of a sudden, I noticed how emotional he was. And I said, what's going on? And that was when he actually told me what he had discovered. And it was heart wrenching, and I was just so upset.
The answer that we got was you don't have to travel far. You've got the very, very, very best in your backyard. They said, Universe of Chicago's got this amazing program. And there's a doctor there by the name of Dr. Everett Vokes, who is breaking ground, who is number one in his field, and he is your guy.
For all we can tell, it had a good outcome because we were able to minimize surgery. And he is here doing important work for us here at the University of Chicago.
Oh, wow, honestly I really love the team there very, very much. I remember that the nurse, the main nurse at the time, Denise, she was absolutely wonderful. Just any questions that we had, they would answer immediately. I got a call from an advertising agency out of New York.
They had a hospital, who they couldn't speak about yet because the client [INAUDIBLE] because we hadn't had the job yet. But they wanted me to do a campaign for them that would help bring recognition to this hospital. A little known to them, I had just left this hospital. I had just been cured of stage four cancer from this hospital. And once they found that out, just the serendipity that coincidences just became a natural.
[INAUDIBLE] frames per second.
Yes, sir.
Let's burn some film.
What we really want to show is that the University of Chicago, first and foremost, has probably some of the best doctors in the world. They are getting the best of the best, and that's what we wanted to show in these spots, that you are dealing with the most innovative technology possible to me. And you're going to come out the other end, and you're going to get right back to your life, and you're going to enjoy your life.
Try to enjoy life to the fullest. I mean if we could travel somewhere just for a day, if we could take a road trip somewhere, we'd do it. And we do it together.
You learn to make every minute count. Every bit of time with your wife, your children, your grand children become more important. I knew at this point that it was time for me to really take the challenge and push everything to the limit and do the absolute best work I could do.
What a nice man Sandro is. He's just a--
He's amazing.
--a good guy. And his wife Claudia is fantastic as well. So it's nice to see that they're doing well. And while we treat some very famous patients, we treat a lot of folks from all walks of life here. And I don't know. If you just had some thoughts on the program in general after seeing the video, if you want to let us know.
One thing that I'd like to point out is that Sandro talked about the fact that he had stage four cancer. And a lot of times when people hear stage four cancer, they're really afraid. They think that this is the end of it. And for head and neck cancer that's really not the case.
In many instances, we have a real high chance of curing this cancer. And I think that's why it's important that folks come to a Medical Center like University of Chicago for treatment because it is quite complex.
Yeah, Dr. Pearson I imagine you stressed that to your patients-- get in, see a physician, and let's take a look at this. What do you see when people come in? Are they afraid? Do they put it off? What do you see generally?
We see-- I think we see a mix of-- we see some patients who have found their cancers just right away, very early. And then another maybe, group of patients that have wanted to minimize that their cancer may have been a problem for some time and present with more advanced cancers. Sometimes cancers that have just been found are harder to treat than ones that may have been around for some time. But it's really important to come and be evaluated so that we can gather all the information about an individual's case.
And Trisha, if you can talk to us a little bit-- and one of the things that I mentioned, that was mentioned in the video, Claudia, I think, talked a little bit about the various people that were involved in the care of her husband and how helpful that was. And truly, we have a multidisciplinary system here. How important is that?
I think it's vital. It's a pretty complicated process getting somebody through treatment from diagnosis all the way through recovery, which is hopefully five years after treatment is completed. So here at University of Chicago, we have a multidisciplinary team that involves medical oncology, ENT surgery, and radiation oncology. And we all have different members of the teams that are responsible for those specific spots.
But we work together as a team to get somebody through that process from diagnosis to recovery five years later. My role is as a nurse navigator. So I'm a person that is there as a contact for patients. I think Sandro's wife mentioned Denise, who was a nurse navigator in our program.
And basically, we're the person that-- we're the people that will help get you through, make sure that everything's on time and on target and all of the teams are working together. It can be a little overwhelming if you were trying to get through that on your own as a patient.
Yeah, I can't stress how important that is because anybody who has been in the health care system and tried to navigate through the complexities of the health care system-- it's a bit of a maze, and it can be very overwhelming, particularly if you're fighting a significant illness. So having somebody like you, there to help them really makes a huge difference. And I've heard it time and time again from patients that the nurse navigators are kind of-- in part they're heroes as they walk their way through the system.
Well, I like--
Not to minimize the doctors.
No, [INAUDIBLE].
[LAUGHTER]
I like to tell people that the doctors are the big picture people. Like they're the ones that put their brains together and their heads together to make sure that we're doing the right thing and the best thing for the people that come to us here at University of Chicago. But the nurse navigators and the nurses and the other teams and ENT and radiation oncology, we're the detail people. So we're the ones that are going to be sort of a first contact and also to make sure that those nit picky details are managed. We're the ones that take care of that.
Now we want to encourage our viewers, if you have any questions, please just type them in the comments section. We'll get to as many as possible here in the next 15 or 20 minutes. So let's ask, here got a question for you. Do all types of head and neck cancer exhibit the same symptoms?
Great question. So I think there are symptoms that are shared. I would say there are symptoms that are shared by all types of head and neck cancer. But they may not.
There's a wide range of different presenting symptoms. It might be a sore that doesn't heal in your mouth. It might be a lump in your neck. It could even be a headache that doesn't go away after some time. We see patients that end up coming into our clinic that have a variety of different symptoms that initially typically are evaluated by their primary care doctor, potentially by an ear, nose, and throat specialist initially before they're referred to our head and neck cancer sub specialty multidisciplinary team.
And we had another pretty famous patient a few years back. And again, he's been used in advertising so we can talk a little bit about him. We wouldn't do this if otherwise. We take our patient privacy very, very seriously here.
Very seriously.
But this was a gentleman who was a very famous chef here in town. And he had, I believe it was tongue cancer. And I can't even imagine having that type of cancer in that line of work. And he's doing great today. So it's exciting to see some of the fantastic advances that have been made in this area. You guys are working miracles it seems like.
Yeah, and I think we take our model of being at the forefront very seriously here at U Chicago Medicine. I think one of the things we really have invested in over a long period of time is an emphasis on clinical research and bringing new ideas to our patients as early.
Yeah, well, and that's one of the tremendous advantages. And I feel like I'm kind of lucky in my line of work. I get to see a lot of interesting things throughout university in the medical center. And people don't realize we're more than just a hospital here. We do have laboratories. We do a lot of research as you said. So kind of the old comment is from the bench to the bedside, we do a lot of things that are trials here. And people can really experience these treatments first that way. So it's very positive.
Got a couple of questions coming in from viewers. First one's more of a statement. A family member was hospitalized and had a mass removed that was blocking her windpipe. And as a temporary tracheostomy and is awaiting biopsy. Just wanted to listen and get more information. And thanks to both of you for providing information.
Is this type of cancer inherited? That's an interesting question.
That's a really good question. And the answer is, it depends. It's not a very satisfying answer, but for the most part, the majority of our patients don't have an inherited head and neck cancer. There is not a-- this is not-- head and neck cancers typically are not part of the overall syndrome that can be passed from father to son or mother to daughter, for example, as is sometimes talked about in other cancers like breast cancer. But there are certain factors, which may be run in families, potentially a-- I think some people are thinking about a susceptibility to viruses such as the human papillomavirus, which might be familiarly related.
Interesting. So one of the things, Tricia, when you were talking a little bit about the multi-disciplinary efforts that we have here that popped in my head too, we do truly cover people from start to throughout their diagnosis and then afterwards as well. And I, again, another area that I was pretty fortunate to see, we have an area within the hospital where cancer patients can come and get help with nutrition and exercise and that sort of thing. And again, these are things that are vital to patients that you may not see other places.
Yeah, I was just touched on our main team's meeting medical oncology ENT surgery and radiation oncology. But we do have a lot of ancillary support as well, which is what you're talking about. We have a dietitian that works very closely with our team.
We have social work. We have physical therapy. And there is a physical therapy area right in our area. We have a special chemo pharmacy that's right on our floor where we do our infusions. And we also have an American Cancer Society representative here on site, and they work very closely with our teams as well as with our social worker. So I feel like we have a lot of support services that are available for our patients.
And I think that's really important to know that you're going through this and you have your family hopefully and the people around you that are supporting you at home, but hopefully, also, you realize that we have a lot to offer you as far as support goes here.
Just to jump in on that, I think we-- in addition to what Tricia said also, our swallowing specialist--
Oh, jeez, how could I forget that apology?
Our symptom management--
Apologies.
--subspecialists. And the other I think important thing about our multidisciplinary team is that we all get together every week face to face and have a talk about every patient issue that's coming through our clinic. That actually happens.
This morning before--
This morning.
--people we're at work, we were in our team meeting--
7 AM.
Yep-- talking. And all of the representatives from all of those teams are present to make sure that all of the issues that are important to receive care across all of these different disciplines were present and could-- can talk. So I think that's a really, really meaningful component.
Oh, I agree. You mentioned your swallowing specialist. And you talked a little bit about the dietitian as well. And in particular, for this kind of cancer, obviously, a swelling specialist is very important. But cancer in general, dietitian's are important because it changes pretty dramatically how you can eat basically.
Exactly.
And that's huge.
It's an enormous deal for particularly the head and neck cancer. We're treating cancers that are located between a patient's mouth and their stomach. And so nutrition is vital and having appropriate nutrition is important for chemotherapy to work. It's important for wound healing. And so having those-- having the access to that nutritional component is effectively sub specialist in that nutritional component is a huge deal to us and our clinic patients.
And we have another question from one of our viewers. Are there any side effects of the HPV vaccine? There can be side effects in general. The side effects from HPV vaccines in general are mild and are related as much to the vaccine delivery as to the vaccine itself. These would be similar to your flu vaccine that you're hopefully getting on an annual basis. But that would be--
Good plug.
Yeah.
[LAUGHTER]
Pain at the injection site, small potential for allergic reaction, and our hope is a major decrease in your risk of HPV related cancers in the long run.
Great. Great. So let's talk about oral cancer treatment. What are some of the things that patients need to know?
Well, I think the most important thing is to come in and talk with your multidisciplinary treatment team about what is entailed. The treatment-- the reason why a multidisciplinary team is so important for head and neck cancer is that our treatment sometimes involve chemotherapy, radiation therapy, or surgery, and/or some mix of all of those over potentially months long periods of time.
Correct.
So developing the plan that's right for you as a patient and your goals as a patient can be complicated, and that's why we emphasize the communication within our medical team so much. So everyone is going to have a different treatment potentially and may or may not have clinical trials that are available to-- for their specific cancer.
And you must be a bit of a mind reader because our next question from our guest was do you have to have chemo or can you have radiation only? But of course, it depends on what's happening to you. It depends on what's happening to you, the specifics of your cancer, your goals as a patient, all of these things weigh into our ability to recommend the best course of treatment to hopefully curing your cancer.
Great. So what are the next steps after being diagnosed with metastatic squamous neck cancer?
Well, I think the most important thing is that whoever has diagnosed the metastatic squamous cell cancer of the head and neck should make sure that you as a patient are hooked up with a team that knows what to do with that diagnosis. So if it's a primary care doctor that's made that diagnosis, we suggest referral to physician or physician teams that are able to put a plan into action.
And if I can jump in here--
Yes.
There is also a difference between metastatic head and neck cancer that's locally metastatic, meaning it's only spread to the lymph nodes in your neck. It hasn't gone potentially to your lungs or your bones or other places in your body. So that's a real important distinction because if it's really just locally, what we call locally metastatic, meaning it's really only confined to the head and neck, we have a real good chance of curing that as well depending on multiple factors. But that is still considered a curative type of disease.
If it's metastatic to other places, then things potentially change. So I think it's important that you know that difference . And that sort of goes back to when people talk about having stage four cancer. It means different things in different kinds of cancer.
I want to say I had a funny look on my face a minute ago. It had nothing to do with your answer. We need to get some sound proofing in here though. It seems like there's all kinds of stuff going on next door. I hope that's not coming over the screen. So we'll keep our fingers crossed. So talk about metastatic cancer of the throat. What exactly is that?
And just to follow what Tricia said, one of the things we get asked a lot is I have cancer of the throat that has metastasized to my lungs, or involves my lungs or my bones. Does that mean I have bone cancer and lung cancer, or does that mean I have a throat cancer? And the answer is that from our perspective as scientists, the cells themselves started in the throat and maintain the same characteristics as they travel to other organs in the body. So those cells, in other words, the treatments that are effective for head and neck cancer remain effective for head and neck cancer whether it's locally in the remains in the throat or in the mouth or has traveled to another place in the body.
Interesting. Now that I would have never guessed because as it hits other areas, I thought maybe that would be a little different. But interesting. So you use the same basic treatments there.
We oftentimes. Many of the treatments are available for a number of different indications, whether the cancer is curable, which we hope, or incurable. And so we-- mostly it's whether or not cancers-- head and neck cancer cell will die if we give say a radiation dose or a chemotherapy treatment course.
Or pluck it out.
Or pluck it out. And that would work whether anywhere in the body we hope that the cancer is located.
Interesting. So let's-- can we talk a little bit more about clinical trials. You touched on it earlier. But I think it's very interesting particularly here at Chicago Medicine. We do a lot of that kind of work. Can you kind of guide us through what's happening and maybe what people can expect if they--
Right, it's an extremely exciting time to be a head and neck cancer researcher because I think we've had just a boon in terms of the number of clinical trials and the number of new types of therapies that are becoming available to us. I think one of the things that we have really been looking at is trying to deploy minimally toxic treatment for HPV positive and HPV negative cancers, and sometimes that means organizing the way we administer chemotherapy and/or immunotherapy in combination and then responding or allowing the tumor to guide us in terms of what next courses we have to administer after that first round of chemotherapy and radiotherapy potentially.
Another question from our viewer--
I'm sorry.
Go ahead. Absolutely.
Can I just-- I just to clarify.
Absolutely.
This is Dr. Pearson's peak. So one of the things that we're looking at and potentially curative cancer in a clinical trial is finding what Dr. Pearson said, but also what we're looking at is trying to find ways that we can potentially cure people with less toxic treatment. So that could mean less radiation therapy, that could mean surgery followed by no radiation therapy. So there's a lot of exciting things that are happening. And it all depends on the number of criteria that would determine whether you would be able to qualify for some of those less toxic type of cures, or less toxic type of treatments working towards potential cure.
Which-- and it's a great point I think because I think people do get frightened when they hear of cancer treatments. You mentioned the chemotherapy and the toxic cures. And you see so much of this stuff on the internet, which you don't read 99% of it and people that are afraid of the legitimate treatments. So they go another way and end up hurting themselves, and it's a shame.
Yeah, there is. I think there was recently kind of an [INAUDIBLE]-- from the scientists among us, there was recently a paper that describes some of the potential harm that patients are incurring in large populations by not pursuing medically or medical oncology directed therapy upfront and looking at other alternative options at the detriment. So certainly we are open to anything that is going to help our patients. But we want to be-- we try to be pretty accurate about what is-- where the evidence is to support the decisions that we would give to our patients.
Yeah, rely on science because that's really what's going to help in a situation like this. A couple more questions from viewers I want to get to. We're getting close to the end of our time. But this is so good. I want to keep it going for at least a few more minutes. Is there a test for HPV in the throat to detect precancerous cells like there is for precancerous cells in the cervix?
So I think that was an interesting question.
It's a great question. Yeah, it's actively under evaluation and investigation. But it's not ready for prime time yet.
Not there yet.
It's coming I think, but it's-- we-- the answer is no right now. But soon, probably.
Interesting. So robotic surgery capabilities, UChicago Medicine. That's another question that we've had. What can you do for people with head and neck cancer?
Yes, and I'm a medical oncologist. So I don't use a scalpel. I use chemotherapy. So I'm not the most accurate person that UChicago Medicine to answer this question. But I'll do my best, and that is that we have a robotic head and neck surgery and ear, nose, and throat surgical machine using the robot. And my surgical colleagues have trained in that, and they're experts at using that.
We have both clinical and non clinical trial and non clinical trial approaches for using that robotic machine to pursue head and neck cancer directed surgeries to hopefully cut out the primary site. But that really-- in order to say whether an individual is a candidate, it requires the evaluation by your ENT, or your ear, nose, and throat doctor.
[INAUDIBLE]
Not every patient is going to be a candidate for using or for having robotic surgery as a-- to cure their head and neck cancer.
So we have one final question. We're out of time. But I want to ask [INAUDIBLE] anyway. And Tricia, I want to start with you on this. So there is a real fear I think people have of cancer coming back. And certainly understandable. What is the single biggest thing that you would want to tell them? And then doctor I want you to get your thoughts on it as well.
So I think I would share with you the fact that we keep a very close eye on our people after they're done with treatments. We make sure that they are monitored with scans, with physical exams as well. So we see patients frequently for the first year after treatment. We see them probably every three to four months minimally, and that's-- it's obviously much more intense, right, after they're done with treatment. But then we'll start to space things out.
In the second year, we generally see people every six months, and then it's annually after that. But we do scans, and we do physical exams. People are seen by medical oncology, their ENT surgeon, and also our radiation colleague. Radiation oncology colleagues as well. So they follow up long term with the Team. Dr. Pearson?
And that's another time where we talk about a lot of those patients in our multidisciplinary head, neck cancer tumor board. We did some of that this morning. I think our anxiety level it's not the same over that follow up period, meaning that most head and neck cancers show themselves within the first couple of years after your initial diagnosis. And so that's when we keep the closest track of patients in there. And the areas, which we think are at highest risk for having cancer has come back. And then up to that five year period where when we've-- when patients have risks, the risk patients having their cancer come back has decreased down to the same level as before their cancer diagnosis.
And so it's at that point where they're as likely to get a cancer of a different type than they are to have their head and neck cancer come back when we kind of released them to their primary care doctor to do the regular screening examinations.
That's fantastic. That was great information.
Thank you.
Thank you.
I have one question, Tim.
Go right ahead.
For the first comment that was from our viewers, there was a question, or more of a statement of their family member is in the process of getting worked up and has a temporary trach. Is there a way for that person to get in touch with us, or will that--
Yeah, absolutely. And that's one of the things I want to point out to viewers too. When you leave the comments, and if we have questions that we didn't get to, we'll try to answer those, and you can certainly take a look at that and send them a message if you'd like to.
Sure.
We can certainly do that.
Well, thank you.
Thank you.
It was great. That's all the time we have for At The Forefront Live. I want to thank our viewers for the great questions. So if you want more information about some of the health topics we discussed on today's program, please visit our website site at UChicagoMedicine.org or you can call 888-824-0200.
Join us for our next At The Forefront Live Thursday February 26th when we will discuss prostate cancer and some of the latest treatments available. Also check out our Facebook page for future At The Forefront Live dates and subjects. Thanks for watching and have a great week.
Request an Appointment
We are currently experiencing a high volume of inquiries, leading to delayed response times. For faster assistance, please call 1-855-702-8222 to schedule your appointment.
If you have symptoms of an urgent nature, please call your doctor or go to the emergency room immediately.
For Referring Physicians
To refer a patient for head and neck cancer care, please call UCM Physician Connect at 1-800-824-2282.
* Indicates required field

Cancer Care Second Opinions
Request a second opinion from UChicago Medicine experts in head and neck cancer care.

Participate in a Clinical Trial
UChicago Medicine head & neck cancer experts are actively conducting clinical trials of new and promising treatments.

Helping You Cope With Cancer
Our Supportive Oncology program offers a range of services to support you and your family during your cancer treatment.
