Cancer Immunotherapy
Harnessing the Immune System to Fight Cancer
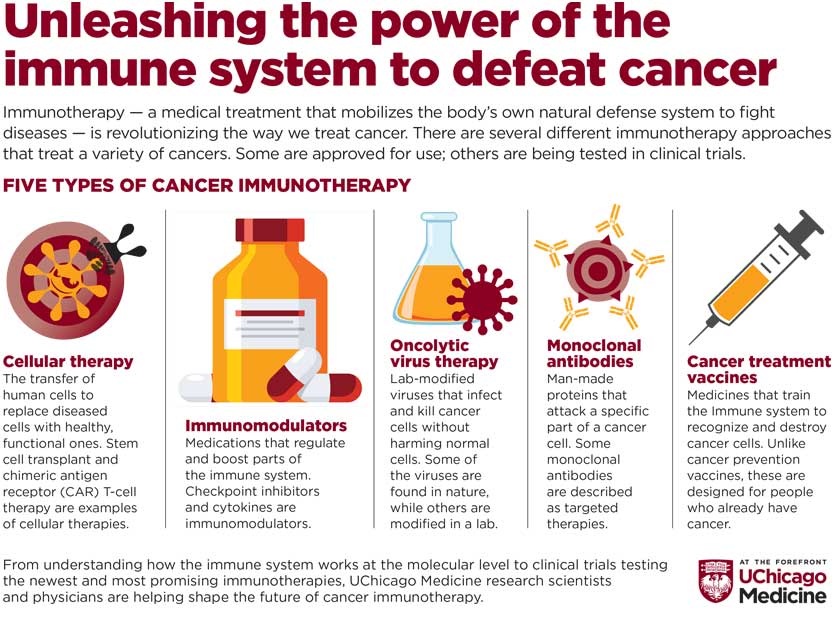
Your immune system protects you from infection, illness and substances that can harm your body. Immunotherapy refers to a medical treatment that turns the power of the immune system against disease. Cancer immunotherapy acts on the cells of the immune system to seek out, recognize and attack cancer.
Types of Cancer Immunotherapy
Several types of immunotherapy are approved for use to treat cancer or are being studied through clinical trials. The different kinds of immunotherapies work in different ways to treat cancer. Some boost the immune system to work against cancer, while others train the immune system to seek out and attack cancer cells.
Cellular Therapies
The transfer of human cells to replace diseased cells with healthy, functional ones. Stem cell transplant, CAR T-cell therapy and tumor-infiltrating lymphocyte (TIL) therapy are examples of cellular therapies.
Immunomodulators
Medications that regulate and boost parts of the immune system. Checkpoint inhibitors and cytokines are examples of immunomodulators.
Oncolytic Virus Therapy
Lab-modified viruses that infect and kill cancer cells without harming normal cells. Some of the viruses are found in nature while others are modified in a lab.
Monoclonal Antibodies
Man-made versions of immune system proteins, designed to attack a specific part of a cancer cell. Some monoclonal antibodies are described as targeted therapies.
Cancer Treatment Vaccines
Medicines that train the Immune system to recognize and destroy cancer cells. Unlike cancer prevention vaccines, these are designed for people who already have cancer.
Clinical Trials
UChicago Medicine physicians lead immunotherapy clinical trials for the following types of cancer:
- Bladder
- Blood
- Leukemia (acute lymphoblastic leukemia)
- Lymphoma
- Multiple Myeloma
- Breast
- Gastrointestinal
- Head and neck
- Liver
- Lung (non-small)
- Melanoma
- Mesothelioma
- Ovarian
- Solid tumors
Immune-Related Adverse Events Clinic for Immunotherapy Patients
Cancer immunotherapies supercharge the body’s immune system to fight cancer. This activated immune system sometimes can lead to unintended side effects known as immune-related adverse events (IrAEs). See how UChicago Medicine's dedicated IrAE clinic provides patients with care and resources unequaled in the region.
