Vulvar Cancer
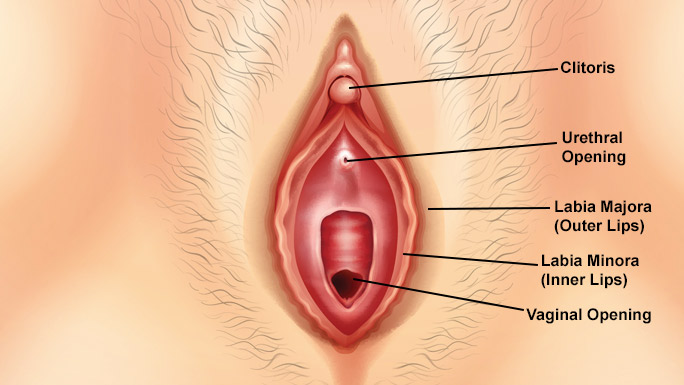
When vulvar cancer strikes, women are often in shock and scared. Many patients don’t know that cancer can affect the vulva, which is the outer part of a woman’s genitals. Women may be worried about their sexual health in addition to the cancer.
Working together, our team of specialists will recommend a treatment plan aimed at curing a woman’s cancer as well as helping her to preserve or regain her sexual function. We also embrace innovative treatments, including clinical trials of new medicines and surgical approaches to reduce side effects and speed recovery.
A number of factors can increase a woman’s risk of developing vulvar cancer:
- Being older than age 50
- Carrying the human papilloma virus (HPV), a common infection that is transmitted sexually or through skin-to-skin contact. There are many types of HPV. Types linked to vulvar cancer include HPV 16 and HPV 18.
- Having a precancerous condition of the vulva called vulvar intraepithelial neoplasia (VIN).
- Having a condition called lichen sclerosus, which can cause the skin on the vulva to become thin and itchy
- A history of cervical cancer or precancerous cervical conditions
- Having a rare skin disease called vulvar Paget’s disease, which causes redness and scaliness.
Vulvar cancer does not always cause symptoms in the early stages. That’s why it’s important for women to get regular pelvic exams. During the exam, the gynecologist will check the vulva for any abnormalities. Women can also get an HPV test as part of a pelvic exam to see if they carry the HPV virus.
Women should also see a doctor if they experience any signs of the following symptoms, which may be signs of vulvar cancer:
- Itching around the vulva that doesn’t go away
- A burning feeling or other pain in the vulva
- Any bumps, lumps or other growths
- A sore in the vulva that doesn’t heal for a month or longer
- A change in color or texture (for example, a part of the vulva appears lighter, darker, or thicker than the area around it)
- Unexpected bleeding or discharge.
When vulvar cancer is suspected, we typically conduct a biopsy, or remove a small piece of suspicious tissue. Our experienced pathologists, who are specially trained in diagnosing gynecologic cancers, use various laboratory tests to determine if the cells are cancerous and what subtype of vulvar cancer it is. There are four subtypes:
- Squamous cell carcinomas: Most vulvar cancers begin in the squamous cells, which are the primary type of skin cells.
- Adenocarcinomas: About 8% of vulvar cancers are adenocarcinomas. These start in gland cells.
- Melanoma: About 6% of vulvar cancers are melanomas, which is a skin cancer that grows in pigment-producing cells.
- Sarcomas: About 2% of vulvar cancers are sarcomas, which start in tissue, bone and muscle cells.
- Basal cell carcinoma: While very rare, basal skin cancer can form in the vulva.
We may also conduct imaging tests, including MRIs and CT scans, to determine how far the cancer has spread and gain other critical information needed to guide treatment.
Surgery
Surgery is the most common treatment for vulvar cancer. Our highly experienced gynecologic-oncologists are experts at operating on the vulva and surrounding organs and tissues. Our primary goal is to remove the tumor, along with a small amount of tissue around it to prevent the cancer from coming back.
If the cancer has spread extensively, part or all of the vulva may need to be removed. This procedure is known as a vulvectomy.
When women are concerned about the appearance of the vulva, our gynecologic-oncologists will partner with plastic and reconstructive surgeons at UChicago Medicine. Our plastic surgeons are experts at taking skin and tissue from other areas of the body to reconstruct the vulva. Reconstruction closes the wound, helps with healing, and provides a semblance of normality.
Our surgeons place a high priority on preventing or limiting pain and other complications from surgery. For instance, not long ago, many women who underwent vulvar cancer operations had numerous lymph nodes in the groin removed to see if cancer had spread beyond the vulva. These procedures sometimes led to lymphedema, which causes chronic leg swelling and other problems. Today, whenever possible, our surgeons use a less invasive approach called a sentinel lymph node biopsy. This involves injecting dye into the cancerous tumor during surgery. The dye naturally travels to the first (or sentinel) lymph node. The surgeon then removes the sentinel node to check for cancer. If the sentinel node is clear, no other nodes need to be removed.
Chemotherapy and Other Drug Therapies
Patients with vulvar cancer may benefit from chemotherapy, which are cancer-fighting drugs.
Women with rare subtypes of vulvar cancer, including melanoma, may also benefit from clinical trials being conducted at UChicago Medicine on immunotherapies, such as Keytruda® (pembrolizumab). Immunotherapies can help the body’s own immune system fight the cancer.
Radiation Therapy
Radiation may be recommended before or after surgery for vulvar cancer. At UChicago Medicine, our experienced radiation oncologists aim to prevent or limit damage to healthy cells and surrounding tissue during radiation. This helps reduce irritation and other side effects.
Patients with vulvar cancer typically get external beam radiation, which is delivered from outside the body. At UChicago Medicine, we use a radiation technique called volumetric modulated arc therapy (VMAT). This technology allows us to deliver radiation to the tumor as well as cancer cells that might be hiding nearby while limiting harm to nearby organs, such as the bladder.
Supportive Services
Our dedicated supportive oncology program provides a range of services, including mental health counseling and social work services. Patients with vulvar cancer and their patients can access these services at any time.

Top-Ranked Cancer Care and High Performing in Gynecological Cancer Surgery
According to U.S. New & World Report's 2024-2025 rankings, UChicago Medicine is the top-ranked cancer hospital in Illinois and high performing for gynecological cancer surgery.
Learn moreMany Women Have Never Heard of Vulvar Cancer. Here's What a Survivor Would Like You to Know
“If I can help one other person to learn what vulvar cancer is, to recognize it, to take care of themselves and make sure they go to the right specialist – then I’ll feel like I’ve given something back to women who may be suffering from this cancer," says Susan Golden, vulvar cancer survivor.
Convenient Locations for Gynecologic Oncology Care
Request an Appointment for Cancer Care
We are currently experiencing a high volume of inquiries, leading to delayed response times. For faster assistance, please call 1-855-702-8222 to schedule your appointment.
If you have symptoms of an urgent nature, please call your doctor or go to the emergency room immediately.
For your convenience, you can make a virtual visit appointment with a cancer expert in the following ways:
– Schedule a virtual video visit to see a provider from the comfort of your home
– Request an online second opinion from our specialists
To refer a patient for cancer care, please call UCM Physician Connect at 1-800-824-2282.
* Indicates required field
