Gallbladder & Bile Duct Cancer

Gallbladder and bile duct cancer affect fewer than 10,000 people in the United States each year. Because these cancers are relatively rare, it’s important for patients to get care at a center with expertise in treating these conditions.
At the University of Chicago Medicine, our approach to treating gallbladder and bile duct cancers is a multidisciplinary one.
Our team includes experts from multiple specialties, including surgeons, hepatologists, interventional and diagnostic radiologists, interventional gastroenterologists, medical oncologists and radiation oncologists. Our program offers a comprehensive and detailed evaluation, bringing together the expertise needed to provide personalized care for every patient.
We see patients with early and advanced-stage disease. And our physicians are equipped to handle complex cases, offering hope for those who have not been considered previously for curative options.
Our physicians are actively involved in research and have made important advancements in diagnostic and therapeutic endoscopic and surgical techniques.
Patients at our clinics receive access to novel treatment options, including the latest clinical trials of promising therapies. Clinical trials span various targeted therapies (such as drugs targeting IDH1 and FGFR, which are frequently found in gallbladder and bile duct cancers) as well as immunotherapies.
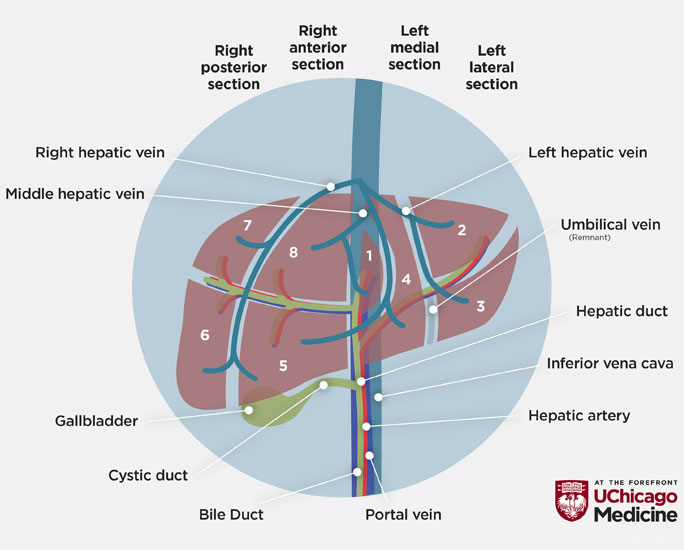
The gallbladder is a small, pear-shaped organ just beneath the liver. It stores bile, a fluid produced by the liver to help digest fats. After a meal, the gallbladder releases bile into one main bile duct (the common bile duct), which carries the fluid into the small intestine.
Gallbladder and bile duct cancers begin in the lining of these structures. The tumors are usually adenocarcinomas — tumors that form in mucus-secreting glands. A common type of bile duct cancer, called cholangiocarcinoma, begins in the bile ducts either inside or outside the liver.
In most cases, gallbladder and bile duct cancers develop in patients who are older, usually in their 60s or early 70s. They are more common in women than men.
Risk factors for gallbladder cancer include:
- Gallstones and inflammation of the gallbladder. Most people with gallbladder cancer also have gallstones or chronic inflammation in the organ. However, most people with gallstones do not develop gallbladder cancer.
- Gallbladder polyps
- Obesity, high-carbohydrate or low-fiber diet
- Family history of gallbladder cancer
Risk factors for bile duct cancer include:
- Primary sclerosing cholangitis, a disease that causes scarring of the bile ducts
- Other chronic liver diseases, including damage from alcohol overuse
- Ulcerative colitis
- Smoking
- Diabetes
- Chronic Hepatitis C
- Congenital (present at birth) bile duct problems
- Some parasites (liver flukes) found in raw or undercooked fish. Liver fluke infection is rare in the U.S., but can affect people who travel to Asia.
Gallbladder and bile duct cancer frequently cause few or no symptoms until they are advanced or have spread to other parts of the body.
Gallbladder cancer is sometimes diagnosed during surgery to remove gallstones.
Jaundice, a yellowing of the eyes and skin that can occur when a tumor blocks the bile duct, is often the first sign of bile duct cancer. About half of patients with gallbladder cancer have jaundice.
Other symptoms of gallbladder and bile duct cancer can include:
- Abdominal pain
- Bloating
- Fever
- Itchiness
-
Loss of appetite
- Nausea or vomiting
- Pale stools
- Swelling in the abdomen or legs
- Tiredness
- Unexplained weight loss
- Weakness
If gallbladder or bile duct cancer is suspected, your doctor will conduct a clinical examination. Blood tests can indicate if levels of liver enzymes or bilirubin are too high, which could be signs of cancer or other disease in the bile duct or gallbladder. Other tests necessary to confirm a cancer diagnosis may include:
- Ultrasound: To identify an obstruction or tumor in the bile ducts and find a mass or tumor associated with the gallbladder.
- Computed tomography (CT): To detect a tumor inside the gallbladder or bile duct and show if it has spread outside of the organ to the liver, bile duct or nearby lymph nodes.
- Magnetic resonance imaging (MRI): To create more detailed images of the liver and bile ducts than a CT or ultrasound can provide. An MRI can show if a tumor is only in the gallbladder or has spread to the liver.
- Endoscopic ultrasound (EUS): Involves a flexible tube, equipped with a camera and other tools, that is passed down through the mouth, esophagus and stomach into the small intestine. The scope uses sound waves (ultrasound) to non-invasively examine the bile duct, gallbladder and surrounding lymph nodes without surgery. If necessary, EUS can help obtain biopsies of tissue to help confirm a diagnosis or can be used to drain or decompress a blocked bile duct or gallbladder.
- Endoscopic retrograde cholangiopancreatography (ERCP): Similar to endoscopic ultrasound, ERCP also involves a flexible tube, equipped with camera and other tools, passed down through the mouth, esophagus and stomach into the small intestine. This procedure, performed by an interventional endoscopist, provides direct access to the inside of the bile duct and can show if it is block or narrowed. During ERCP, the endoscopist also can take a tissue biopsy or provide endoscopic therapy directly to the tumor.
- Surgery: To determine if cancer is in the gallbladder or bile duct and to take a tissue sample for biopsy.
- Biopsy: Is the final step in determining an accurate diagnosis of gallbladder or bile duct cancer. Tissue from the tumor and a bile sample may be taken through a needle guided by a CT scan, during an ERCP or during surgery. A pathologist will examine the tissue and/or sample under a microscope.
Treatment for gallbladder and bile duct cancer depends on the type and stage of the tumor, the patient’s overall health and the chance of curing the disease or extending the patient’s life.
Surgery
Surgery is the most effective treatment for gallbladder and bile duct cancers and offers patients the best chance of cure. Surgical procedures include:
- Cholecystectomy: For very early stage tumors confined to the lining of the gallbladder. This surgery involves the removal of the gallbladder. For more advanced tumors, the gallbladder is removed and nearby lymph nodes and part of the liver may also be removed.
- Bile duct surgery: For tumors confined to the bile ducts. This surgery involves the removal of the bile duct and nearby lymph nodes.
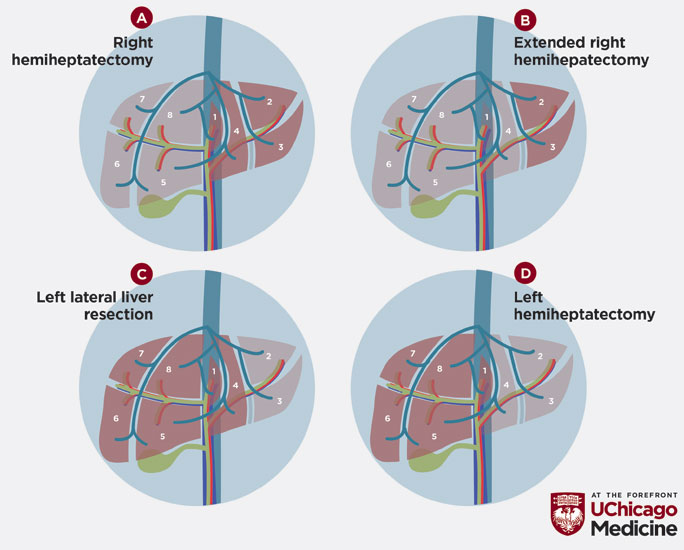
- Partial hepatectomy: For large bile duct tumors inside the liver. This procedure involves removing part of the liver (a wedge of liver tissue, a lobe or a larger portion of the organ).
- Whipple procedure: For bile duct tumors that are close to the pancreas (known as extrahepatic or distal tumors). This procedure involves the removal of the gallbladder, the bile duct, the head of the pancreas, part of the stomach and part of the small intestine.
- Hepatic artery infusion (HAI) pump chemotherapy: For bile duct tumors that have spread to the liver (metastatic bile duct cancer, intrahepatic cholangiocarcinoma), HAI is a powerful treatment that shrinks liver tumors and reduces the risk for tumor recurrence.
- Liver transplant: Patients with certain types of cancer, including intrahepatic cholangiocarcinoma and hilar cholangiocarcinoma, may be candidates for liver transplant. Our transplant oncology team is highly skilled in determining when transplant may be the best option.
Minimally Invasive Procedures for Symptom Relief & Treatment
Patients with gallbladder and bile duct cancer are not candidates for surgery if the cancer has already spread at the time of diagnosis or due to the location and severity of the cancer. Image-guided, minimally invasive procedures to help drain bile out of the gallbladder or a bile duct can relieve some symptoms such as pain, jaundice, nausea, vomiting and infection. These procedures may be performed through a laparoscope or through an endoscope or under radiology guidance.
Endoscopic-directed therapy options also are available for patients who are not surgical candidates. UChicago Medicine's interventional endoscopy program is one of the few centers that can provide non-surgical, endoscopic methods to treat unresectable or recurrent tumors, including radiofrequency ablation (RFA) or photodynamic therapy (PDT). In patients with persistent symptoms including jaundice, pain or obstructed stents, these therapies can prolong the time to recurrent symptoms or obstruction and in some cases, may increase survival.
Chemotherapy
UChicago Medicine medical oncologists find innovative ways to integrate chemotherapy with each patient’s multidisplinary treatment plan. For patients who may become candidates for surgery, we integrate chemotherapy with local-regional therapies (such as TARE/Y90) to achieve maximum disease control, while allowing for the “future liver remnant” (remaining healthy liver tissue after surgery) to grow, to make surgery possible. This approach can potentially convert inoperable tumors to operable tumors. In this situation, the goal of chemotherapy is to eradicate early “micrometastases" — dangerous “cancer-initiating cells,” which can be hiding elsewhere in the body even before surgery. When a patient has advanced or metastatic gallbladder or bile duct cancers, chemotherapy may be used to slow tumor growth, relieve symptoms and extend survival.
In addition to traditional chemotherapy, we are actively investigating newer approaches of systemic therapies (including targeted therapy and immunotherapy) for patients with gallbladder and bile duct cancers. Please refer to the Clinical Trials section for more information.
Radiation Therapy
Radiation therapy can be used in three different settings for gallbladder or bile duct cancer:
- Before or after surgery, in order to eliminate tumor cells and improve the chance of cure with surgery
- As “definitive therapy” for unresectable disease
- For palliative care to help improve symptoms that the tumor may cause
Most commonly, radiation is given on consecutive days over several weeks in conjunction with chemotherapy.
UChicago Medicine radiation oncologists use advanced radiation techniques to treat gallbladder, bile duct and other gastrointestinal cancers. Treatments include:
- Intensity-modulated radiation therapy (IMRT): Delivers high doses of radiation more precisely than conventional radiation therapy. Subsequently, normal tissues can also be better protected, enabling higher doses aimed at the tumor.
- Stereotactic body radiation therapy (SBRT): Delivers a course of treatment in five days or less, using advanced methods of tumor targeting to facilitate much higher daily doses of radiation.
At UChicago Medicine we have a vast array of technology for immobilizing and targeting tumors. In conjunction with pre-treatment placement of markers in select cases, these approaches can be used to provide pinpoint accuracy.
Clinical researchers at UChicago Medicine actively investigate new therapies for gallbladder and bile duct cancers, including targeted therapy and immunotherapy options. Our oncologists are pioneers in this area — often among the first to offer certain experimental treatments for the disease. As a result, our patients have the opportunity to participate in several institutional and national/international gallbladder and bile duct cancer clinical trials.
We are at an unprecedented era of discovery, where our new knowledge of disease biology has led to the development of promising new therapeutic strategies. Examples of current clinical trials include targeted therapies against genomic alterations such as IDH1, FGFR and HER2 in bile duct cancers, and a combined radiation and immunotherapy strategy for both advanced gallbladder and bile duct cancers.
Hepatic Artery Infusion (HAI) Pump Chemotherapy for Liver Metastases
The hepatic artery infusion pump is a wireless metal pump that is placed inside the abdominal wall during a surgical procedure. The device is about the size of a hockey puck. The pump is connected to the liver via a small tube placed into a blood vessel connected to the hepatic artery.
The HAI device pumps high doses of chemotherapy directly into the liver-- as much as 300 to 400 times higher than intravenous chemotherapy. The high doses of medication remain in the liver as opposed to circulating through the body as in traditional therapy.
Over time, tumors shrink or disappear. For patients who are not yet candidates for surgery to remove tumors, HAI can shrink tumors so they can be removed with surgery. For patients who have had liver tumors removed, HAI can reduce the risk of tumor recurrence.
The UChicago Medicine Comprehensive Cancer Center is one of a select number of hospitals in the nation that offers this advanced treatment. We're also leaders in hepatic artery infusion research, and are actively conducting clinical trials, with the goal of making HAI available to more patients who may benefit.
Learn more about hepatic artery infusion and request an appointment at UChicagoMedicine.org/hai.
Convenient Locations for Cancer Care

Cancer Care Second Opinions
Request a second opinion from UChicago Medicine experts in cancer care.

Center for Endoscopic Research & Therapeutics
The Center for Endoscopic Research and Therapeutics uses the most innovative minimally invasive techniques to treat a range of gastrointestinal problems.

Participate in a Clinical Trial
UChicago Medicine cancer experts are actively conducting clinical trials of new and promising treatments.
