How can you tell if your IBD is getting worse?

If you are like many people with inflammatory bowel disease (IBD), you have good days and bad days. Those bad days could be a sign that your Crohn’s disease or ulcerative colitis is becoming more active. But even on the good days, your IBD could be “silently” active without you knowing it.
What are some warning signs that IBD is active?
Some people with IBD may have clear signs of disease relapse, also known as a “flare.” Signs of active Crohn’s disease or ulcerative colitis include:
- Blood or mucus in the stool
- Abdominal pain
- More frequent bowel movements
- Greater urgency to have bowel movements
- Rectal pain during bowel movements
Other signs of active IBD specifically in people with Crohn’s disease include:
- Nausea
- Vomiting
- Bloating
IBD can also cause symptoms that affect other parts of your body, such as:
- Joint pain and stiffness
- Eye inflammation
- Skin rashes
Many people with IBD have some of these symptoms when their disease is active, but others do not. In some, there could be a lag time of several months between the time their disease becomes active and the development of symptoms. So, it is possible to have a disease relapse and not realize it.
Intestinal ultrasound can detect IBD relapse weeks — if not months — before symptoms occur.
That’s why proactive disease monitoring is so important when you have IBD. It enables you and your doctor to adjust your treatment before you have pain, urgent bowel movements and other uncomfortable symptoms, halting the progression of your disease and other poor outcomes.
What are some common reasons for disease relapse in IBD?
Unfortunately, we don’t understand all the reasons that lead to disease relapse. Some of the causes we know of include:
- Stopping or skipping doses of your IBD therapy
- Living with active disease
- Antibiotics
- Pregnancy
- Stress
How does stress make IBD worse?
We know there is a bidirectional connection between the brain and digestive system called the gut-brain axis. It’s like a road with traffic going both ways. What happens in your gut affects your brain and vice versa. People with active IBD are more likely to experience stress, anxiety and depression. Conversely, stress, anxiety and depression can aggravate IBD symptoms.
Understanding the gut-brain axis is a top priority for physician-researchers at UChicago Medicine. We hope to find new ways to manage IBD by studying this connection.
Is there a way to know if my IBD is getting worse before a disease relapse?
Yes. Regular monitoring can help prevent your disease from becoming active. Through proactive monitoring, we can measure inflammation before you feel symptoms. This allows us to act on it, so you spend more time in remission — and less time dealing with IBD symptoms — and avoid complications.
Some of the ways IBD specialists at UChicago Medicine proactively monitor your IBD include:
- Stool or blood tests that measure inflammation
- Endoscopy, during which the doctor inserts a small flexible tube with a camera into the mouth or anus to evaluate your bowel. Biopsies can be obtained with this test.
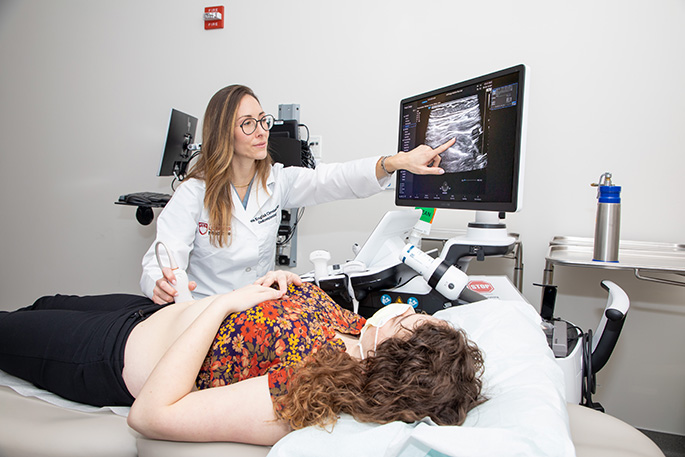
- Intestinal ultrasound, the latest IBD monitoring option, which does not require any preparation and is performed in clinic by placing an ultrasound probe on your abdomen.
The University of Chicago Medicine Inflammatory Bowel Disease Center is one of only a few IBD centers in the country — and the only one in the Midwest — to offer intestinal ultrasound to IBD patients.
What are the benefits of intestinal ultrasound for people with IBD?
Intestinal ultrasound is the latest in treatment for Crohn's disease and ulcerative colitis. This accurate, reliable technology can detect disease relapse weeks — if not months — before symptoms occur.
Intestinal ultrasound can show how well an IBD treatment is working for you as early as two weeks.
An intestinal ultrasound can verify if you are experiencing a relapse by displaying in real time what is happening inside your gut. Then, you and your doctor can talk about how to modify your treatment so you feel better faster.
Intestinal ultrasound is also convenient. It doesn’t require any advance preparation like fasting or “bowel prep.” It is also painless and does not involve any radiation. It takes about 20 minutes or less to complete.
How do doctors at UChicago Medicine use intestinal ultrasound to monitor IBD?
Your IBD specialist may recommend that you have intestinal ultrasounds regularly to monitor your disease. By providing highly accurate images of your bowel, an intestinal ultrasound can measure the degree of active inflammation. Your doctor can use this information to assess changes since your last visit.
Your doctor may also suggest having an intestinal ultrasound after you start a new therapy to check how your body is responding. Research suggests that intestinal ultrasound can show how well a treatment is working for you as early as two weeks. So, if a treatment isn’t controlling your inflammation, your doctor can quickly adjust your care plan.
How do I get an intestinal ultrasound?
Your UChicago Medicine IBD specialist can determine if intestinal ultrasound would be beneficial for you. If so, one of our specially trained gastroenterologists can perform an intestinal ultrasound during your regular clinic visit.
Your doctor will apply gel to your abdomen and use a small probe to inspect the interior of your intestines during the procedure. The results are immediate, so you and your doctor can discuss whether changing your treatment regimen would improve your symptoms.
By offering this advanced technology at UChicago Medicine, we aim to help you achieve remission faster and remain in remission.

Noa Krugliak Cleveland, MD
Dr. Krugliak Cleveland specializes in gastroenterology and serves as Director of the Intestinal Ultrasound Program at UChicago Medicine.
Learn more about Dr. Krugliak Cleveland