Uterosacral Ligament Suspension
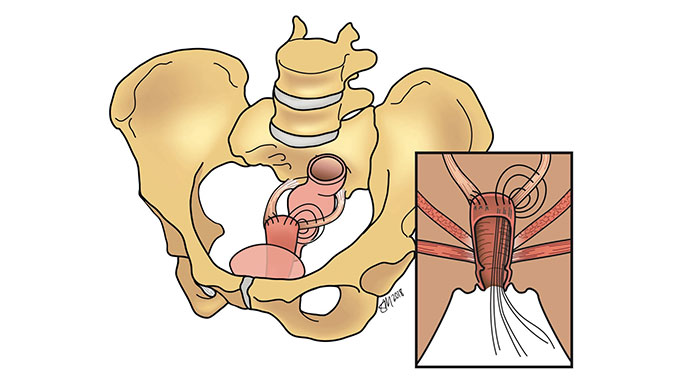
This procedure helps to correct vaginal vault or uterovaginal prolapse. Uterosacral ligament suspension surgery is very similar to sacrospinous ligament suspension surgery except the urogynecologic surgeon will stitch the top part of the vagina to the uterosacral ligaments instead. This is a “native tissue repair,” meaning the urogynecologic surgeon will use the patient’s own tissues to restore and support the vagina after prolapsing.
This surgery can be performed at the same time as a hysterectomy or can be performed in women who have already had a surgical procedure.
How is this surgery performed?
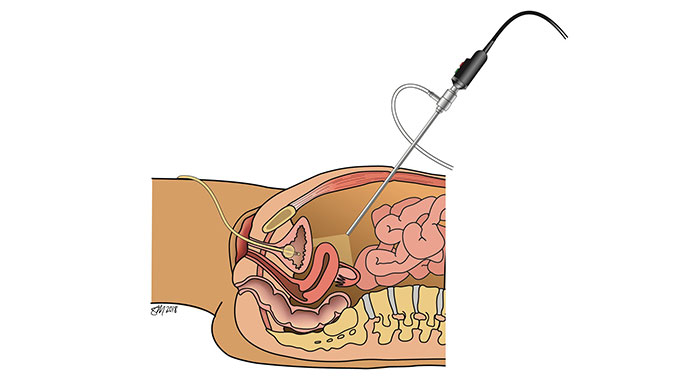
A uterosacral ligament suspension is performed through a minimally invasive abdominal approach utilizing either conventional laparoscopy or robotic assistance or through the vagina. In either approach, the top part of the vagina is sewn to the ligaments with permanent and or delayed-absorbable stitches. This type of prolapse procedure is referred to as a “native tissue repair” because your own tissue is used to restore the support of the vagina. Scar tissue will then form around the stiches, further helping the vagina to stay in place.
How successful is this surgery?
This procedure has been extensively researched and is a good surgical option for treating vaginal or uterovaginal prolapse. However, since the patient’s own tissue is used to help make the repair, women who choose this surgery have a higher risk of recurrent prolapse and might require another surgical procedure in the future.
What are the complications?
Outcomes and complications for uterosacral ligament suspension have been extensively studied, including:
- Bleeding/hematoma formation at the surgical site
- Lower back/buttock pain
Although rare, some women develop pain during sexual activity after surgery. If this occurs, your urogynecologist can refer you to a pelvic floor physical therapist to alleviate your symptoms.
What does recovery look like?
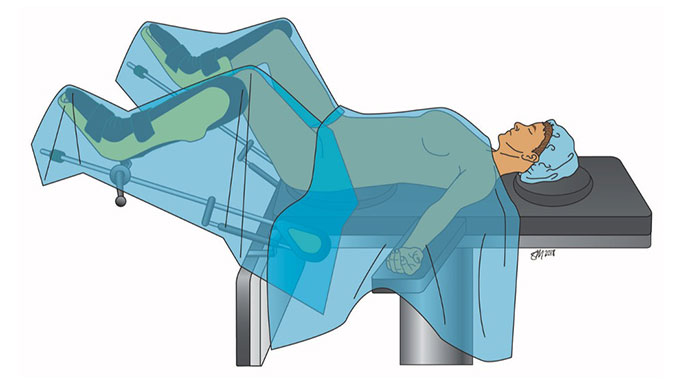
Owing to the minimally invasive approaches used by your University of Chicago Medicine urogynecologic surgeon, you will be able to go home the same day as surgery.
Enhanced Recovery After Surgery (ERAS) Program
To help you properly heal and get back to do the activities you love, our urogynecologists have developed an Enhanced Recovery After Surgery (ERAS) Program to reduce post-operative pain, nausea and fatigue. As quality-of-life surgeons, we are passionate about restoring your quality of life, and aim to return you to the activities that you find interest in as quickly as safely possible. We allow you to resume activity as you see fit, listening to your body and its response to physical activity. However, we do ask you to refrain from sexual activity for several weeks while the stitches in your vagina heal. Most women feel back to normal within two to four weeks following surgery.
Meet Our Urogynecologists

Urogynecology and Reconstructive Pelvic Surgery

Urogynecology and Reconstructive Pelvic Surgery

Urogynecology and Reconstructive Pelvic Surgery

Urogynecology and Reconstructive Pelvic Surgery

Urogynecology and Reconstructive Pelvic Surgery
