UChicago Medicine transabdominal cerclage team helps prevent pregnancy losses for hundreds of families each year

Laura Douglass, MD, (left) and Andrew Fisher, MD, learned how to perform transabdominal cerclage from the pioneering gynecological surgeon Arthur Haney, MD. Now they use their skills to help prevent hundreds of pregnancy losses each year.
For Laura Douglass, MD, the retirement of her mentor, the renowned reproductive endocrinologist transabdominal cerclage. He retired in the fall of 2020.
About 1% of women have a condition known as cervical insufficiency, once called incompetent cervix. It causes weak cervical tissue dilates prematurely during pregnancy, leading to premature birth or, frequently, the loss of a pregnancy. Often, the condition is diagnosed after a second trimester pregnancy loss — and for those who have experienced it, the prospect of another is devastating.
“I went through four losses before I found out about cervical insufficiency,” said Alana Scott, of Markham, Illinois. “I didn’t plan on having kids, but I found out I was pregnant and then had a miscarriage almost immediately, and we never talked about it, we just pushed past it.
“After the third time, I knew there was something wrong with me, but I was scared to find out because I didn’t want to go through this ever again — but then boom, I was pregnant again. And when that pregnancy began to fail, even after a transvaginal cerclage, I was transferred to UChicago Medicine, where they told me that they could help figure out what was going on before I got pregnant again.”
There were no treatments for cervical insufficiency until the development of a technique known as the McDonald or transvaginal cerclage in the 1950s. Typically used in cases where a patient is already pregnant and experiencing cervical dilation, the procedure involves placing a band of sutures around the lower part of the cervix, essentially tying it shut. While the transvaginal cerclage has a high rate of success, it doesn’t work for everyone.
An Alternative to Transvaginal Cerclage
During his tenure at UChicago Medicine, Haney championed an alternative treatment: transabdominal cerclage, or TAC. The technique involves surgical placement of a sturdy, woven band around the top of the cervix, which supports the weight of the growing pregnancy and prevents the cervix from opening prematurely.
“I like to use a balloon analogy,” said Andrew Fisher, MD, Assistant Professor of Obstetrics and Gynecology at UChicago Medicine. “If you think of the uterus as a balloon expanding as it fills, a transvaginal cerclage is like pinching the bottom of the balloon and holding on until eventually it gives way. But if you tie a string higher around the base of the balloon, it’ll hold that pressure for much longer.”
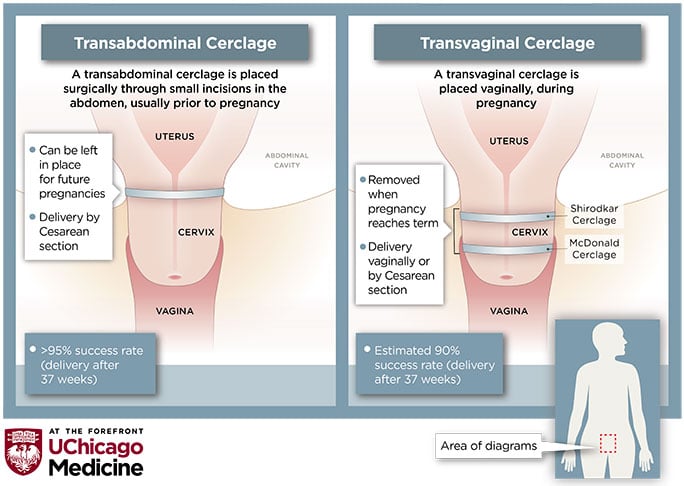
TACs are usually placed prior to pregnancy and are permanent. Individuals with a TAC in place must deliver via a scheduled C-section, and the band can be left in place for any future pregnancies. At UChicago Medicine, the procedure is over 95% successful allowing for a late or full-term delivery (meaning delivery occurs at 36 weeks of pregnancy or later).
Q&A: Pregnancy, fertility and childbirth with transabdominal cerclage (TAC)
The procedure is challenging and rare: Most hospitals may conduct only five or 10 such surgeries each year. But thanks to Haney’s legacy, UChicago Medicine conducts hundreds of TAC procedures annually.
It’s important for this procedure to be conducted at a center of excellence, by people who place them frequently.
The Transabdominal Cerclage Program is led by Douglass, Assistant Professor of Obstetrics and Gynecology, and supported by Fisher, who came to UChicago Medicine in June 2020 to train with Haney prior to his retirement. Their focus is on growing the support team and empowering patients to understand their options.
“We’re not just teaching a bunch of people how to do this procedure just because it’s uncommon,” said Douglass. “We feel strongly that if someone is going to do this, they need to be a good gynecological surgeon. It’s important for this procedure to be conducted at a center of excellence, by people who place them frequently.”
Because cervical insufficiency is rare, and providers offering TAC are rarer still, patients come to UChicago Medicine from around the world for the procedure. The team has found that the pandemic-induced shift toward telemedicine has made screening and preparing patients much easier.
“Many patients have already discussed cerclage with their providers, so by the time we see them for a consultation, they’ve done their homework,” said Douglass. “The shift toward video consultations during the pandemic has been a huge boon. We can go over a patient’s records and discuss the pros and cons of doing this procedure, because it’s not the right fit for everyone. Being able to talk to patients virtually and make that connection is fantastic.”
In Scott’s case, it was a whirlwind decision to have the TAC placed.
“UChicago Medicine took me in when I was about seven weeks pregnant, and Dr. Douglass said we needed to place the cerclage by nine weeks,” she said. “So, my husband and I dove into the information we had and saw that it had a long recovery period — it wasn’t a guarantee that the baby would reach term. But we decided we had run out of options, and if this could help save the baby, then it’s a no-brainer.”
Complications of TAC are rare and typically are related to inexperienced surgeons. “It’s easy to do this procedure badly,” said Douglass. “You need to be really sure you’re getting great placement to get a good result. But for us, the surgery is straightforward, because we know what to do and how to put them in.”
What’s next for the TAC program?
As the program at UChicago Medicine continues to grow, the team hopes to develop a research program focused on understanding which patients are the best candidates for TAC and which patients should be watched closely for potential complications.
“Historically, we have great results with this procedure, and we’re not interested in changing the recipe,” Douglass said. “The biggest thing will be analyzing our historical data to determine how well this procedure works for patients from different populations, of different ages, with single or multiple births. We’d also like to see what we can do to make the recovery from this surgery easier on patients and make it more of an outpatient procedure.”
Fisher and Douglas also hope there will be broader awareness among other healthcare providers about TAC as an option.
“I don’t think physicians talk enough with one another or their patients about how traumatic it is to experience repeated, pre-viable pregnancy loss,” said Fisher. “I think that’s the biggest risk for most of our patients, and their biggest concern. Everything is on the line for them. Surgical risks exist, but those are rare when you compare it to the likelihood of going through this trauma again without an intervention like this. Patients need to know that this is an option, and that we’re here to help.”
Ultimately, the goal of the TAC program remains the same: making sure that loving parents can finally bring home a baby.
For Scott, it was all worth it.
If I hadn’t come to UChicago Medicine, I would never have known TAC was available. It saved my son’s life.
“At 37 weeks of pregnancy, on December 23, I went in and had a C-section, and everything went as planned,” she said. “I still have the cerclage, though I don’t think we’ll have another child. Everything that I went through and fighting so hard for my son, I don’t think that mentally I could handle another pregnancy.
“At the end of the day, I’m very happy I met Dr. Douglass. I owe her a lot. She helped my husband and me get through this. If I hadn’t come to UChicago Medicine, I would never have known TAC was available. It saved my son’s life.”

Laura A. Douglass, MD
Gynecologic surgeon Laura A. Douglass, MD, is the director of the Transabdominal Cerclage (TAC) Program. In addition to TAC surgery, she also has advanced expertise in robotic, laparoscopic and hysteroscopic procedures.
Learn more about Dr. Douglass
Andrew Fisher, MD
Andrew Fisher, MD, specializes in obstetric and gynecologic medicine and treats a wide range of conditions affecting women, including abnormal uterine bleeding, opioid use disorder in pregnancy, hormone therapy for gender affirming transgender patients and more.
View Dr. Fisher's physician bio