Strokes & other neurovascular conditions: What you need to know

Understanding common and complex neurovascular issues can help prepare you to react in the event you or a loved one experiences a sudden neurological emergency. As internationally recognized neurovascular experts, we have answers to common questions about conditions affecting the brain and spinal cord.
What is an acute stroke?
Strokes occur when the blood flow to an area of your brain is blocked, preventing oxygen and nutrients from reaching your brain tissue. This can happen very suddenly, in the case of an acute stroke. Brain cells are very fragile, and begin to die within minutes.
The symptoms of stroke include numbness or weakness in the face and limbs, especially on one side of the body; sudden confusion; trouble speaking and difficulty understanding others; sudden difficulty seeing and walking; and sudden severe headache.
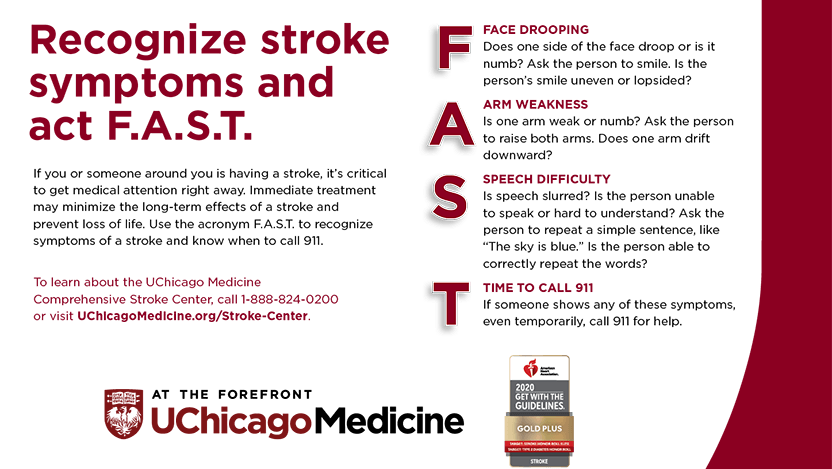
If you are worried someone may be having a stroke, we recommend using the F.A.S.T. test:
F — Face: When you ask the person to smile, does one side of their face droop?
A — Arms: If you ask the person to raise their arms, does one arm drift downward?
S — Speech: If you ask the person to repeat a simple phrase or talk to you, is their speech slurred or confused?
T — Time: Act fast. If you see any of these signs, call 911 right away.
There are three primary types of strokes, and they can have different causes.
The first type, called an ischemic stroke, occurs when blood flow to the brain is blocked, often due to a blood clot. Most strokes fall into this category (87%).
The second type of stroke, the Transient Ischemic Attack (TIA), is also often caused by a blood clot. These “mini-strokes” occur when blood flow in the brain is only blocked for a short time. TIAs are considered warning signs of future strokes that could occur within hours to days after the TIA.
The third type of stroke is known as a hemorrhagic stroke. These occur when an artery in the brain leaks or ruptures, putting pressure on the surrounding brain cells and causing damage. These can be caused by high blood pressure and weakened blood vessels, including conditions such as aneurysms, arteriovenous fistulas and arteriovenous malformations.
Lifestyle factors can also contribute to risk of stroke, such as high blood pressure, high cholesterol, smoking, obesity and diabetes. Other medical factors include heart disease, medications or conditions that can alter sex hormone levels, sleep apnea, age and ethnicity.
What causes brain aneurysms? Who is at risk?
Brain aneurysms, or cerebral aneurysms, are weak spots found on the arteries of the brain that fill with blood and bulge out. The bulge can put pressure on surrounding brain tissue, causing damage, and it can also rupture, causing a hemorrhage, which can cause a hemorrhagic stroke.
An unruptured aneurysm does not usually cause symptoms, unless it is pressing on other brain tissue. This pressure can cause pain behind the eye, facial paralysis, numbness and weakness, changes in vision and a dilated pupil. Unruptured aneurysms still carry a significant risk for bleeding in the brain.
Ruptured aneurysms can cause symptoms such as an extremely severe headache, nausea, vomiting, double vision, seizures, loss of consciousness and cardiac arrest.
The weak spots in the brain’s blood vessels that lead to cerebral aneurysms can be congenital, meaning they are present from birth, and may be the result of inherited risk factors, such as genetic tissue disorders or arteriovenous malformations. Lifestyle and health associated risk factors can include untreated high blood pressure, smoking, drug use, and age.
Not all aneurysms will rupture; risk factors that contribute to aneurysms rupturing include the size and shape of the aneurysm, the aneurysm’s location and a family history of aneurysms. Smoking and high blood pressure also increase the risk that an aneurysm will rupture.
What is an arteriovenous fistula or malformation? Is it life-threatening?
Arteriovenous fistulas (AVF) and arteriovenous malformations (AVMs) are unusual connections between the body’s arteries and the veins. Normally, blood travels from the arteries to the capillaries in tissues like the brain, where the blood can deliver oxygen and nutrients. With an AVF or AVM, the blood bypasses the capillaries and goes directly into the veins due to tangled blood vessels. They are extremely rare (present in less than 1% of the population) and are usually congenital (meaning a person is born with it) but rarely inherited.
AVMs (or AVFs) in the brain are not always life-threatening, but they can present unique risks. These abnormal blood vessel tangles are often weak, which can cause blood leakage and aneurysms. Patients with AVM (or AVF) frequently experience brain hemorrhages, seizures, headaches and other neurological challenges.
Brain bleeds, such as those that can occur due to an AVM or AVF, are extremely dangerous and can cause hemorrhagic strokes. However, they can be treated with minimally invasive surgery, and bleeds can be prevented with lifestyle changes, such as avoiding excessive exercise.
Can you recover from an acute stroke?
Stroke recovery is possible, especially if a person receives rapid medical care. Emergency care is critical, even if the symptoms resolve quickly. If someone is showing symptoms, call 911 immediately. Paramedics can help recognize stroke, stabilize patients who are at risk of immediate complications from stroke such as blocked airways, and transport patients to stroke centers to receive emergency treatments proven to reduce death and disability from stroke.
After a stroke, patients may continue to experience paralysis and weakness on one or both sides of the body, difficulty speaking and cognitive and emotional challenges.
Recovery depends on severity of the stroke, how quickly medical care is received, and rehabilitation resources available to the patient after the event. For the best care, patients should look for a Comprehensive Stroke Center. This designation is awarded to institutions that demonstrate dedication to evidence-based medicine and advanced treatment options for individual, complex patients.
UChicago Medicine is one of 10 Joint Commission-certified comprehensive stroke centers in the state of Illinois and the first to be designated in Chicago. From the prestigious neuroendovascular suite to the specialized neurocritical care and neuro-stroke units, we provide comprehensive, individualized care to help our stroke patients recover and achieve the highest quality of life possible. Our physicians work as a team to evaluate each unique case and determine the best treatment approach. As an academic medical center, we are also involved in a wide range of stroke research projects, working to develop new medications and treatments for preventing and treating strokes.

Shyam Prabhakaran, MD, MS
Shyam Prabhakaran, MD, is the Chair of the Department of Neurology at UChicago Medicine. He is an internationally recognized leader in vascular neurology and stroke research and treatment, and has led projects focused on uncovering the underlying causes of recurrent strokes, improving stroke care, and optimizing patient outcomes and recovery.
See Dr. Prabhakaran's bio
Tareq Kass-Hout, MD
Tareq Kass-Hout, MD, is an expert on strokes and other neurovascular conditions at UChicago Medicine.
Learn more about Dr. Kass-HoutStroke Center
The University of Chicago Medicine is a Joint Commission Certified Comprehensive Stroke Center, nationally recognized for its expertise in providing the highest level of care for stroke patients.
Learn more about our stroke and neurovascular services