First-of-its-kind medication shows promise for liver disease patients
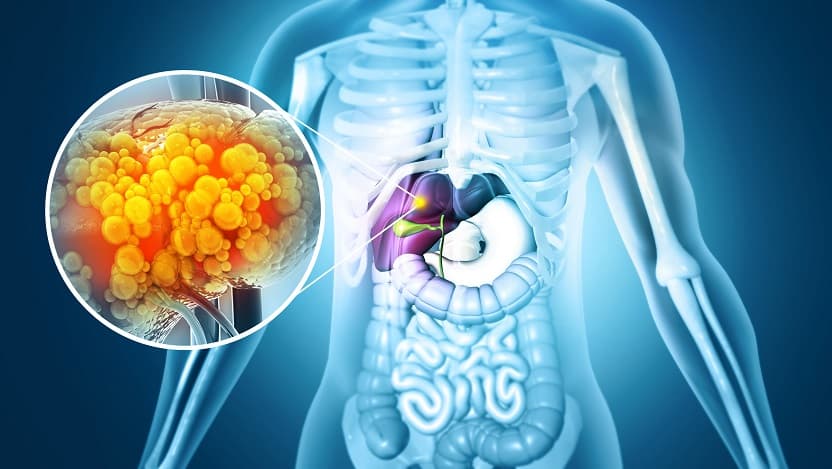
Metabolic dysfunction-associated steatotic liver disease (MASLD) can cause harmful scarring in the liver. For some clinical trial participants, the drug resmetirom improved this scarring or slowed its progression.
Metabolic dysfunction-associated steatotic liver disease (MASLD), formerly known as non-alcoholic fatty liver disease (NAFLD), is estimated to affect nearly one-quarter of adults in the United States. In some people, this chronic condition can cause the formation of liver fibrosis—scarring of the liver—that can even progress to liver failure, making this disease among the most common reasons patients need liver transplants. Yet, as of February 2024, there are no approved drugs doctors can use to treat this disease.
Fortunately, that may be about to change. Researchers at the University of Chicago Medicine contributed to a recent clinical trial of a medication that showed promise in both improving fibrosis and managing associated metabolic imbalances that can lead to cardiovascular issues and other health concerns. The results of the trial were published in the New England Journal of Medicine.
Tackling liver disease from a metabolic angle
The new drug, resmetirom, was initially developed as a medication for lowering the levels of unhealthy lipids in the body such as cholesterol. But scientists, physicians and pharmaceutical experts realized that it had the potential to treat the metabolic issues that lie at the heart of MASLD and drive disease progression to fibrosis and other negative outcomes.
As the drug progressed through liver disease clinical trials, experts like Mary Rinella, MD, Director of Metabolic and Fatty Liver Disease at UChicago Medicine, provided direction on study design and development.
The recent paper, of which Rinella is an author, reports on a pivotal phase 3 clinical study that followed nearly 1,000 patients over the course of a year.
“This study demonstrated — for the first time in a drug with a good side effect profile — improvement in fibrosis and less disease progression,” Rinella said. “It’s especially remarkable because it was only a year-long study; normally we'd expect it to take years for people to get better.”
Since their metabolisms don’t work properly, patients with MASLD usually have imbalances in the levels of lipids throughout their bodies, not just in their livers. As a result, there is a strong association between MASLD and cardiovascular complications like coronary heart disease and even heart failure. In the recent trial, the researchers found that resmetirom not only improved fibrosis and inflammation in the liver for some patients but also improved lipid levels for some patients.
“That finding was really pleasing,” Rinella said. “Between people whose disease progression halted and those who saw improvements in lipids and fibrosis, about two-thirds of patients had a favorable outcome with resmetirom.”
Since patients who responded favorably to the drug not only showed improvement in existing fibrosis but also a significant reduction in the underlying metabolic “engine” that drives fibrosis, Rinella said the researchers expect those patients to have fewer of the downstream complications normally associated with liver disease. The trial has been extended so the researchers can gather even more data about the drug’s impact on longer-term, liver-related outcomes.
There has been at least one other drug that previously showed potential for treating MASLD, but Rinella said severe side effects were a likely culprit in preventing FDA approval. In contrast, they said resmetirom was so well-tolerated it came as a surprise even to the researchers.
“It’s quite remarkable: we’re used to things like cancer treatments that involve complicated procedures and have a vast array of side effects, but this is a pill taken once a day with very few side effects,” Rinella said.
Looking to the future of MASLD treatment
In light of the dearth of treatments for liver disease, the FDA had previously outlined an accelerated approval pathway for drugs that achieved specific biological improvements or reductions in negative clinical outcomes in patients with nonalcoholic steatohepatitis (NASH), an advanced form of MASLD. Based on the reported results of the trial, Rinella and her colleagues are hopeful that resmetirom will become available in the clinic very soon.
“As soon as it is approved and we have access to it, I anticipate that we’ll be able to start prescribing it to patients,” Rinella said. “It’s being targeted for use by specialists rather than primary care doctors, so UChicago Medicine will be a great resource that can receive referrals from other physicians.”
Rinella also emphasized that the primary treatment for MASLD is still intervention with dietary therapy and behavior modification.
“That needs to be part of the overall approach, regardless of possible drug options,” she said. “One of the things that set UChicago Medicine’s clinic apart is that we have endocrinologists and dietitians embedded in our liver disease care teams to support patients through those changes they need to make.”
Rinella pointed out that many people with MASLD don’t know they have it because it is sometimes asymptomatic, especially if there is no fibrosis yet. Without symptoms, the disease only shows up on clinical tests like ultrasounds, blood tests or CT scans. Now that there might be a drug that could reverse some liver damage and prevent future damage, she said it will be important for clinicians to work even harder to identify those asymptomatic patients.
“Millions of people are out there who could potentially benefit from this drug,” she said.
The study, “A Phase 3, Randomized, Controlled Trial of Resmetirom in NASH with Liver Fibrosis,” was published in the New England Journal of Medicine in February 2024. Co-authors include Stephen A. Harrison, Pierre Bedossa, Cynthia D. Guy, Jörn M. Schattenberg, Rohit Loomba, Rebecca Taub, Dominic Labriola, Sam E. Moussa, Guy W. Neff, Mary E. Rinella, Quentin M. Anstee, Manal F. Abdelmalek, Zobair Younossi, Seth J. Baum, Sven Francque, Michael R. Charlton, Philip N. Newsome, Nicolas Lanthier, Ingolf Schiefke, Alessandra Mangia, Juan M. Pericàs, Rashmee Patil, Arun J. Sanyal, Mazen Noureddin, Meena B. Bansal, Naim Alkhouri, Laurent Castera, Madhavi Rudraraju and Vlad Ratziu, M.D., Ph.D. for the MAESTRO-NASH Investigators.

Mary E. Rinella, MD
Dr. Rinella is an expert in fatty liver disease (steatotic liver disease). She provides comprehensive liver disease assessment and treatment, including nutritional intervention, the use of medications, endoscopy and clinical trials to deliver the most advanced treatment options.
See Dr. Rinella's physician bio