Fatty liver disease diet: What foods help prevent and reverse fatty liver?
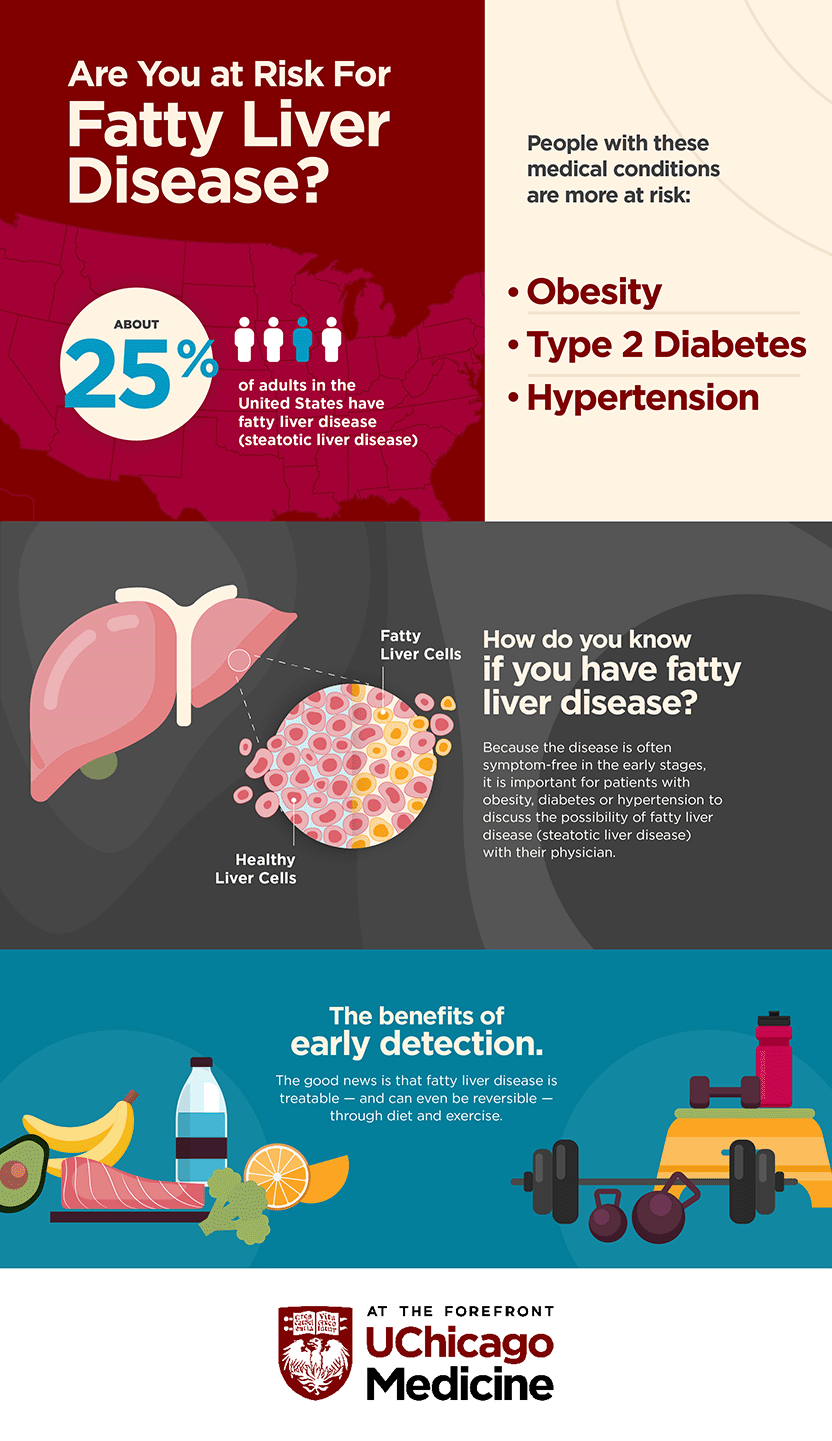
Medical providers preach about the importance of a healthy diet, but nutrition isn’t always one-size-fits-all. For patients with fatty liver disease, the country’s most common chronic liver condition that affects about 100 million Americans and can lead to cirrhosis and cancer, it's important to focus on diet and lifestyle changes.
As a registered dietitian and nutritionist at the University of Chicago Medicine's Steatotic Liver Disease Clinic, I recommend a diet full of healthy fats and plant-based foods – as well as up to three cups of coffee per day – to help keep your liver healthy.
How can I improve my liver health?
According to the American Liver Foundation, there are no medical treatments – yet – for non-alcoholic fatty liver disease. So that means that eating a healthy diet and exercising regularly are the best ways to both prevent liver damage from starting or reverse liver disease once it’s in the early stages. We know people don’t want to feel like they’re on a “diet,” so we work really hard with our patients to help them focus on lifestyle changes instead, which includes a healthy diet, exercise and getting a lot of quality sleep.
What foods help reverse fatty liver disease?
They might surprise you. We recommend patients with non-alcoholic fatty liver disease drink three cups of coffee per day, eat four tablespoons of olive oil a day and follow a Mediterranean diet, which emphasizes eating primarily plant-based foods and healthy fats.
People usually can’t believe we’re asking them to add more food like coffee and olive oil to their diet, rather than restrict items or cut things out.
What is the best diet plan for a healthy liver?
We recommend the Mediterranean diet to our liver patients.
The Mediterranean diet is everything you would expect a dietitian to recommend – more fruits and veggies, more whole grains, more nuts and legumes, lean meats, less red meat and less sweets/added sugars.
Why is the Mediterranean diet the best diet for fatty liver disease?
The Mediterranean diet is a well-known diet that gained popularity in the 1990s, known more as an eating pattern rather than a structured diet. It emphasizes eating fruits, veggies, whole grains, beans, nuts, legumes, olive oil, and flavorful herbs and spices; fish and seafood at least a couple of times a week; and poultry, eggs, cheese and yogurt in moderation, while saving sweets and red meat for special occasions.
In addition to being good for people with non-alcoholic fatty liver disease, the Mediterranean diet has been associated with a decreased risk of heart disease, and it's also been shown to reduce blood pressure and bad LDL cholesterol. And it can be in line with the American Diabetes Association's nutrition guidance. That’s important because both heart disease and diabetes are strongly associated risk factors for fatty liver disease.
How can a dietitian help patients with fatty liver disease?
A key role the dietitian plays is individualizing the nutrition plan for each patient. Every patient is unique and everyone has different needs.
Adapting to a Mediterranean diet is hard for patients because we are surrounded by convenience foods and junk on a daily basis. This diet is focused. It is important for patients to be able to sit down and learn about the benefits of the recommended diet and ask questions. Then they can set realistic and attainable goals with a nutrition expert, rather than something that sets them up to fail.

Annie Guinane, RD, LDN, CNSC
Annie Guinane, RD, LDN, CNSC, is a registered dietitian and a licensed nutritionist who works at the UChicago Medicine Steatotic Liver Disease Clinic.
Learn more about the Steatotic Liver Disease Clinic