Quadruplet treatment delays the need for stem cell transplantation in newly diagnosed multiple myeloma patients
A clinical trial at the University of Chicago Medicine Comprehensive Cancer Care Center is showing promise in treating newly diagnosed multiple myeloma patients with a four-drug (quadruplet) therapy.
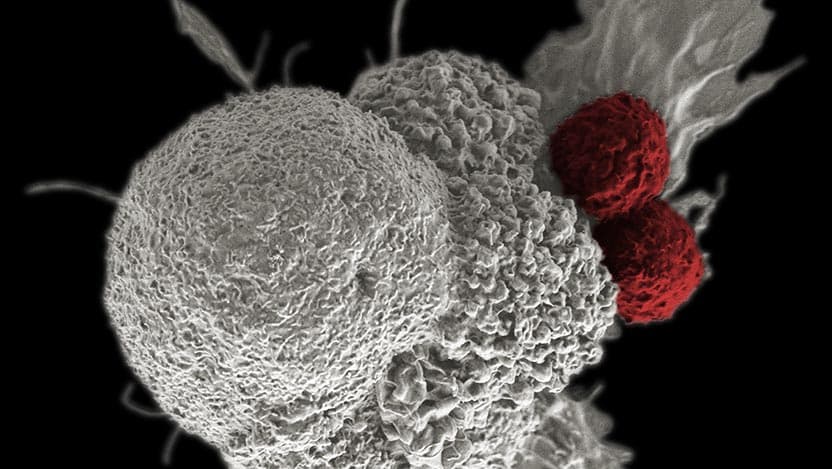
Multiple myeloma (MM) is a rare cancer of plasma cells, a type of white blood cell in the bone marrow that produces antibodies. Treating MM successfully requires several classes of drugs working together and in many cases a stem cell transplant. In a phase 2 clinical trial conducted by physicians at the University of Chicago Medicine Comprehensive Cancer Center, more than half (58%) of patients with newly diagnosed MM had a complete response from a four-drug combination (quadruplet) therapy including the novel immunotherapy drug, elotuzumab, to an existing treatment known as the KRd regimen, which consists of carfilzomib, lenalidomide and dexamethasone.
The results of the "quadruplet" therapy were promising, suggesting that patients might be able to forgo the side effects caused by stem cell transplantation. The results of the study were published in Andrzej Jakubowiak, MD, PhD, senior author of the study. He is also a professor of medicine and director of the myeloma program at UChicago Medicine.
In myeloma, a clone of mutated plasma cells multiplies in an uncontrolled fashion and produces substantial amounts of antibody; growth of these plasma cells, usually in bone marrow, have far-reaching effects on the bones, kidneys, blood count and a variety of other factors. Altogether, it leads to the dysfunction of multiple organ systems. Comprehensive treatment is required to be able to control the disease and possibly eradicate it.
These patients have a 72% probability of being progression-free survival at three years, which is truly among the best results so far.The majority of patients with myeloma are diagnosed in their late 60s or early 70s.
“Myeloma affects the African American population two to three times more than any other race,” said Benjamin Derman, MD, assistant professor of medicine and first author of the paper.
In MM, high doses of a chemotherapy known as melphalan followed by a stem cell transplantation remains the standard of care for transplant eligible patients. While stem cell transplantation can be life-saving and can stop the disease's progression, it also requires 2 to 3 weeks of hospitalization and a difficult 2- to 3-month recovery period, possibly with side effects like short-term diarrhea, loss of appetite, low energy, nausea and vomiting. Several studies have shown that quality of life deteriorates during this period, said Derman.
Moreover, treatment with melphalan has serious delayed side effects such as causing secondary cancers like leukemia. Melphalan treatment is known to suppress the immune system. Combining immunotherapy with melphalan can further suppress the immune system. This increased immunosuppression can lead to high-risk complications if the patient is exposed to infections like COVID-19. Because of the risks associated with chemotherapy and stem cell transplantation, there is a great need to develop alternative treatment strategies for MM patients.
“This is the first time that quadruplet therapy using elotuzumab is being tested in newly diagnosed MM patients. Many people had reservations on whether elotuzumab is strong enough to produce additional effects when added to the triplet regimen, KRd; however, the results presented in this paper look very promising and suggest a positive effect of an addition of elotuzumab to KRd,” said Jakubowiak.
Of the 45 patients included in this study, 48% had genetic abnormalities that made their MM high risk. Irrespective of stem cell transplant eligibility, all patients received 12 cycles of elotuzumab-KRd treatment. To assess the depth of response to treatment, bone marrow aspirate from the patients was tested for measurable residual disease (MRD). The test determined how much disease was left after 8 and 12 cycles of the treatment using a very sensitive technique called clonoSEQ® next-generation sequencing. Based on the MRD results, decisions were made either to de-escalate or continue treating the patients with additional cycles of elotuzumab-KRd.
This is the first time that quadruplet therapy using elotuzumab is being tested in newly diagnosed MM patients.This type of study design is called an MRD-adapted trial because treatment is de-escalated based on the MRD test results. This MRD-adapted trial design allowed patients to stop carfilzomib if the patient achieved sustained MRD-negativity, so that patient was not exposed to extra cycles of therapy which would limit the possible toxicity and also reduce the costs associated with treatment.
Jakubowiak is excited about this study because they achieved impressive results in high-risk patients using MRD-adapted quadruplet therapy. Stringent complete response and/or MRD negativity was achieved in 58% of patients and the estimated three-year progression-free survival and overall survival were 72% and 78%, respectively. Jakubowiak is encouraged by these results because it means some patients will not need to undergo a stem cell transplant.
The authors caution against using MRD status at early time points to determine employment and timing of stem cell transplantation. Furthermore, this study demonstrates that MRD directed de-escalation of therapy without undergoing transplantation can lead to deepening and durable responses. The major criticism of this study was that some of the interventions or de-escalations were not controlled as the study didn’t have a multi-randomized approach; a separate study comparing this approach with KRd alone and/or without de-escalation is recommended to evaluate the effectiveness of MRD-adapted elotuzumab-KRd.
“At this point, we can’t confirm whether quadruplet therapy is superior to triplet with stem cell transplantation therapy in terms of overall survival, nor can we determine if we can completely bypass transplant in newly diagnosed MM patients,” Derman said.
“Stem cell transplantation may be an appropriate option for many transplant-eligible patients, but because of the risks associated with transplantation, there are situations where it may be better to delay or avoid stem cell transplantation, for example if deeper responses can be achieved with novel immunotherapies like this quadruplet therapy,” Jakubowiak said.
Nevertheless, the current study with quadruplet therapy holds promise for future antibody-based combination regimens in transforming the lives of patients with MM.
The study “
Andrzej Jakubowiak, MD, PhD
Andrzej Jakubowiak, MD, PhD, is an internationally known expert on multiple myeloma, a cancer of the plasma cells in bone marrow. He works closely with the Multiple Myeloma Research Consortium (MMRC) to bring the latest treatments to the patient’s bedside as quickly as possible.
See Dr. Jakubowiak's profile
Benjamin Derman, MD
Benjamin Derman, MD, is an expert in multiple myeloma and other plasma cell disorders, such as monoclonal gammopathy, amyloidosis, plasmacytoma and POEMS syndrome. He is actively conducting clinical trials of promising new cancer therapies.
View Dr. Derman's profile