Abdominal Aortic Aneurysm
Abdominal and Iliac Aortic Aneurysm
What is abdominal aortic aneurysm (AAA)?
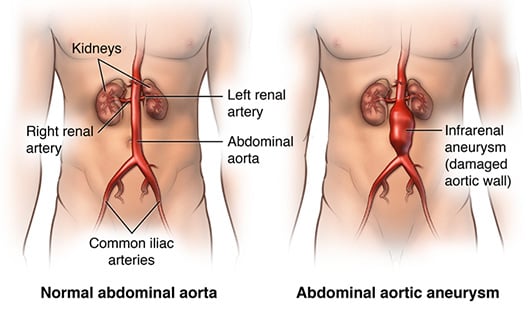
An abdominal aortic aneurysm is a condition that occurs when part of the aorta becomes enlarged. Normally the abdominal aorta is a round circular structure that resembles a pipe, roughly the size of a golf ball. When an aneurysm develops, the aorta expands and its walls become weaker, similar to an expanding balloon. This enlargement puts the aorta at risk for rupturing, which can be like threatening if not treated immediately.
What is an iliac aneurysm (IAA)?
The iliac artery branches off from abdominal aorta into the lower part of the pelvis that directs blood flow to the legs. With an iliac aneurysm, the wall of the iliac artery can expand and weaken, which puts it at risk for bursting. If this happens, it is a life-threatening condition that requires immediate medical attention. It is very common to have iliac aneurysms associated with an aortic aneurysm.
Risk Factors for Abdominal Aortic and Iliac Aneurysms
Though people can experience stomach, back or groin pain to signify a possible aneurysm, often those symptoms are felt only when the aneurysm is close to rupturing and requires immediate emergency care. The best way to prevent a fatal abdominal or iliac aneurysm rupture starts with knowing what risk factors apply to you and how to take active steps to decrease your chances of an aneurysm. Common risk factors include:
- Age: Greater than 50
- Gender: Aortic aneurysms impact men more than women
- Family history: It has been shown that there are higher incidences of aortic disease if one or more family members have been previously diagnosed
- Genetic factors: Certain collagen vascular disorders, such as Marfan Syndrome, Loey-Deitz Syndrome and Vascular Ehlers-Danlos Syndrome, lead to a higher risk of developing aortic disease
- Preexisting aneurysm: A previous aneurysm increases your chances of additional aneurysms
- Lifestyle Threats: The following comorbidities increase the likelihood of you having aortic disease:
- Smoking
- High blood pressure
- High cholesterol
- Diabetes
Prevention for Abdominal/Iliac Aorta Aneurysms
Once you know you are at risk for abdominal aortic and iliac aneurysm, prevention is the most effective way to decrease your changes of having a serious condition. The best methods of prevention are smoking cessation and well-controlled blood pressure. Reasonable physical activity is okay after an aneurysm has been diagnosed.
Ultrasound Scan
If you have a family history of aortic aneurysm, you and the other members of your family are at a higher risk of an abdominal or iliac aneurysm. An ultrasound, a painless, non-invasive, radiation-free test, is the best screening tool for detecting aortic aneurysms. Ultrasound allows us to see and measure the aorta and iliac arteries in great detail, and identify an existing aneurysm so we know how to prevent further complications.
Lifestyle Management
Leading a healthy, or healthier, lifestyle can dramatically reduce your risk of aortic aneurysm. Having regular exams to monitoring your cholesterol and blood pressure can lower your chances of having a severe an aortic aneurysm.
For those who smoke, making the effort to stop smoking is critical for long-term aneurysm prevention. You should also consider joining smoking cessation groups designed to help at-risk patients quit smoking.
Abdominal/Iliac Aortic Aneurysm Treatment Options
UChicago Medicine offers a full range of medical and surgical therapies to treat abdominal and iliac aortic aneurysms with treatment plan focused on our patient’s specific condition. Our approach to personalized care looks beyond just the disease itself to create a plan that centers around your diagnosis, risk factors, size (5 cm in women and 5.5 cm in men), shape and severity of the dissection to deliver safe, effective, customized treatment. Common treatments may include one or more of the following:
- Controlling or modifying risk factors: Quit smoking, control blood pressure, manage blood sugar is diabetic/pre-diabetic to help slow the progression of the aneurysm
- Observation: Routine ultrasound can monitor the size and rate of growth of the aneurysm. A CT scan is frequently obtained if there is growth seen on an ultrasound.
- Medication: Decrease factors such as hyperlipidemia (elevated levels of fats in the blood) and/or high blood pressure
- Open Aneurysm Repair: Replacement of the diseased area of the aorta with a fabric graft
- Endovascular Aneurysm Repair: A minimally invasive alternative to the open repair
- Hybrid Aneurysm Repair: Combination of open surgery and endovascular to repair the aorta
Abdominal aortic aneurysms are more common than most people realize. Basically it's an enlargement of the aorta in the abdomen area. Now sometimes the aorta can burst, which can be life threatening. Jim Craig-- the goalie for the United States hockey team that won gold in 1980-- will be on the program to discuss the condition that took the life of his father.
We'll also have one of the leading experts in the treatment of abdominal aortic aneurysms, that's Dr. Ross Milner. He's the director of the Center For Aortic Diseases at UChicago Medicine. We'll take your questions and answer as many as possible on the program. That's coming up now on At the Forefront Live.
[MUSIC PLAYING]
Now today on At the Forefront Live we have Dr. Ross Milner, director of the Center For Aortic Diseases here at UChicago Medicine. And Jim Craig is joining us. Welcome to both of you.
And quick reminder to our viewers, this show is not designed to take the place of a visit with your health care professional. But we also want to remind people to type in your questions in the comments section. We'll get to as many as possible within the next half hour. Welcome to both you gentlemen. Appreciate you being here.
Thank you.
Yeah, I'm looking forward to it.
Jim, I want to start with you because it's not often that we have a hockey goalie on the show. In fact, you'll be the first. And I guess the question would be, why is this so important to you, and why are you here today?
Well, my father died of a ruptured aneurysm, and it was because he really wasn't aware. And so I was fortunate enough to work with W L Gore in the Ultimate SAAVE Campaign. And then I've been going around the country for the last 12 years helping raise awareness and saving a bunch of lives. So today I'm really, really excited to come back here with Dr. Milner to help all the viewers understand how important it is to be screened.
And Dr. Milner, let's talk just a little bit about-- give a definition first of all so we know what an abdominal aortic aneurysm actually is. If you can tell us what it is, and we'll go from there.
Great, thanks. So an abdominal aortic aneurysm is a ballooning of the normal blood vessel that runs in your abdomen, supplies a lot of the important organs. And when it gets too large or too thin, it's just like a balloon that starts out small and grows. And when it gets too large it can burst. And when that happens, it can be a life threatening event. So we'd like to identify people, as Jim said, before that happens so that we can treat it, so that the aneurysm won't rupture.
And what strikes me-- we were talking a little bit before the program, and this really struck a nerve with me-- is that this is more common than people realize.
It's much more common than people realize. And one of the things that Jim has done so well with his advocacy for awareness is getting people to think about it. And for men at a certain age, and if you have a family history and are a smoker, or have a history of high blood pressure, you're at risk for this disease. And it's very easy to check for, and there's no risk with the screening that can be done. And it can be identified more often, and it's a common problem that isn't checked for often enough.
And Jim, this is your passion. it's. Really important to you, and obviously it started with your father. But you've gone and worked for years now to try to raise awareness. Tell us a little bit about what you've done and what people need to know from a screening standpoint.
Well, as Dr. Milner said, it's the silent killer. You don't have symptoms. And so really awareness has to be the biggest thing. And I'm married now, I have two children. And my dad my mom never got to see them, and it was just because of awareness.
And so when I was fortunate enough to be part of the Ultimate SAAVE Campaign and work with Gore, we have figured out ways through the last 12 years to reach different communities. And that's today Facebook Live is just an awesome way to do that. But also my dad had perfect symptoms. He had high blood pressure, he was a smoker, he had had a massive heart attack at age 45. But as you get older, you need somebody that's an advocate. So people who are out there need to listen and understand how they can help.
And in my case, my dad went to the wrong hospital, went to a small hospital. Didn't even have a vascular surgeon. And he passed away. And today with all the knowledge we have, that probably wouldn't happen. And the great part of all this work has been my brother Don had an aneurysm. We had him checked, and he's been taken care of. So there's a family member. And as Dr. Milner said, this is not only if you're a smoker, but a family history. So it's really up to the viewers today to really pay attention to who they know that was in their family that could have died from a ruptured aneurysm.
In the old days, Dr. Milner, they might have even thought they had a heart attack, right? And so I don't even think ruptures are accurate. I think there's even more than we know about.
Well Jim, you even said before the show-- which again, I thought was interesting-- you were talking about your father. And he mentioned that one of the symptoms he had, he thought he had kidney stones. So describe what he was going through as far as the symptoms. What was he complaining of?
As I've learned from my work with all these great doctors throughout the years is that my father had a contained ruptured, and so it gave false signs. So he went to where he was comfortable. And we didn't know any better. We weren't smart enough, we weren't educated like you guys will be today after this show. And so we brought him where he was comfortable, which was a much smaller hospital. And because there was no vascular surgeon there, there was probably no way of even saving lives.
And the progress in medicine and with these endovascular products that come out-- especially working with Gore and learning and how they use them. Dr. Milner, it's really quite amazing how it's changed from back when my father had an open procedure to what they do today.
And Dr. Milner, talk to us a little bit about the symptoms of the abdominal aortic aneurysm. Because there are things that people can be aware. First of all, who is more prone to have this happen? We've noticed you were talking about smoking, and there are some things to look for. But who's more prone to have it? And then what would the symptoms be?
Sure. So Jim, as both of us have mentioned a little bit already-- so men. Are much more common in men than women. Men over the age of 65. People who smoke. People who have a family history. And people who have high blood pressure are the highest risk.
As Jim said, most of these have no symptoms at all. People feel fine, they don't even know they have the problem. And when we really get concerned are when people have symptoms, because that can be a sign of a ruptured aneurysm. And those symptoms would be abdominal pain or back pain. Or even more concerning at times, someone will just pass out at home and no one knows why. And they're not seen soon enough, and it's because they've lost so much blood from a ruptured aneurysm. And still they could be saved if they got to a hospital. But abdominal pain, back pain, and someone who passes out.
And when we talk about an abdominal aortic aneurysm, one thing that-- again, I think people need to be aware and be educated-- when you think of the aorta, I think most of us think of the heart. This is actually not taking place in the heart, correct?
That's right. Actually, one of the things people ask me all the time, what a vascular surgeon does. And most people think I'm a heart surgeon. And no offense to the heart surgeons out there, but I am a vascular surgeon. So the distinction is an abdominal aneurysm is down in the stomach. There are aneurysms that can happen all over the body, but this is specifically when we talk about a triple A-- or abdominal aortic aneurysm-- is down in the lower part of the abdomen. Down near your belly button just to give you a sense of where that would be. And aneurysms can happen up higher closer to the heart. But specifically what we're discussing are an aneurysm in a lower location.
So Jim, I've got to talk a little bit about-- because I would be remiss, and I'm sure I'd get a bunch of angry notes on Facebook-- I've got to talk a little bit about your background. Because I remember back in 1980, I remember this well, watching your team. It was the miracle on ice. It was a miracle. Walk us through those days, and here you are today advocating for this. So it's been quite a change for you.
Yeah. Sometimes in life you get a platform and you're able to use it to do good things. And when I met Dr. Milner I knew that we had a kindred spirit, and that someday we would do something together that would be really beneficial. What I loved most about being on that team was that we figured out how to be part of something bigger than ourself. And this cause today is so much bigger than myself. I always tell people I want to live long enough to see my kid's kids. And I've just got my first granddaughter.
Oh, congratulations.
And the part about this is if you are aware and you are screened and they find it, these doctor's success rate is like 98%. It's incredible. You go in the hospital and you're in and out in a day. You have this constant care, you get the right hospitals, they're able to monitor you, the product is great. And so to see someone suffer a tragedy like I did with my dad because people are just not aware, it's not good enough.
So our team, the biggest thing that I loved about our coach is he drove change. He figured out a way to win that nobody else had thought of before. And I think that's exactly what you guys are doing today with this Facebook Live. It's just an incredible tool to raise awareness.
So Dr. Milner, I'm curious, you're the director of the Center For Aortic Diseases. So you do this work all the time. And that's important when you want that type of treatment. And you mentioned sometimes there is an issue where maybe somebody will go to the wrong spot. And I don't want to make this a shameless plug, but this is-- and I'm heading that direction-- but this is an area of expertise for you and for the center. And why is that so important?
Yes. This is an area of expertise for us as you said. One of the aspects of it is actually something Jim was just talking about. We have a great team. We have a great team of doctors. We have a great team of nurses in the operating room. We have a great team of nurses in our outpatient clinic. We have anesthesia doctors, we have ICU doctors and the nurses in the floor. We have a really great team of people that can take care of patients.
And I think one of the things that we're very proud of is we've been consistently recognized here for the outstanding care that we provide and have been high performing. Because abdominal aortic aneurysm repair is looked at nationally and is graded in terms of the quality of the care you provide, and we're a high performing center for that with a very high volume. And it's something we're very proud of because we try to take great care of patients, but we do this as a team. And although I have the title of director, I have an amazing group of people that work with me that provide outstanding care to people and save people that potentially wouldn't have opportunities otherwise.
So we've heard a little bit about screening and how important that is. What do you do when you find somebody that has one of these that-- do you immediately work on them, or what happens?
So it depends on the size. Some are more concerning than others obviously. The larger it is the more urgent it is to get care. Usually our first step is the ultrasound, as Jim mentioned with the Ultimate SAAVE Act. The next step is a CT scan so we can determine how the repair can be done, and then make sure it's safe for them to go to the operating room. And sometimes it's within the day if it really is a problem, or even within hours or immediately. And sometimes these are electively repaired depending on the size. But we really make the next step of our decision based on what the CT scan looks like.
And Jim, we were talking about the ultrasound before we got the show going here. And it's such an easy-- I'm not saying it's easy to do an ultrasound-- but it's easy on the patient. Very non-invasive, very simple procedure for the patient, and a lifesaver.
Yes. And I was screened and I always joke. I say, it's a little jelly on your belly. It's that simple. And what happens is most of the people that people find, as Dr. Miller would tell you, is by mistake. They've gone in, they have pneumonia, they've taken an X-ray, somebody noticed it. So for all the primary care physicians that are out there, it's really in your community. And the community is what's really important. That's why we're here, is to really look out for one another and be a little more educated today. You don't have to just look for yourself who might have an aneurysm, you have a chance to look at any loved one, friend, or anybody else, and make them aware of it.
And the ultrasound part is, Dr. Milner, when you know a patient has an aneurysm, you meet with your representatives for the company that you're going to use. You sit there, they study, you work together. It's a really well planned out operation, and the results are amazing.
But when you have a rupture, it's a-- I don't want to use the word-- but it's not a good big. And the results are not normally very good. And even if you do save them, that person doesn't seem the same. So the awareness part is incredibly important.
Yes. And one of the points of when we were talking about this earlier-- which I think is really important-- not just that the ultrasound is technically easy to do-- because it is relatively easy-- it's a completely safe test. There's zero risk to an ultrasound. So when you're looking at a screening test to be checked, there is zero risk to an ultrasound. And you can get it done, and it is easy to know right away if it's something that you need to be concerned about and look into more with absolutely zero risk.
And so you find the aneurysm-- and we were talking about stents also before the program. So explain how that works. And I think, again, most people when they think of a stent, they think of something a little different than what you're doing.
Yes. So we are able to repair a lot of aneurysms now with a less invasive approach. Which as Jim mentioned, people are going home even as early as the next day for a lot of our patients. And it's a procedure that's done through the arteries in the groin, the femoral arteries. A lot of times with tiny, tiny little incisions even that you can't even see that we're able to use to get to devices there. Which is a dramatic change from what was the big standard operation, which was a lot of time to recover from. And although it's a very good surgery, it takes a long time to recover from that. And with the stent approach it's a lot better.
The stents that are used to repair aneurysms, most people think of the stents that are put in the heart, which are small stents, which are about two or three millimeters in size, and are just plain bare metal that keeps the artery open. The way these stents are, they're much bigger, almost 10 times the size of the stents put in the heart. And they have fabric around them so that all the flow goes through the stent and away from the aneurysm. And then what we see over time is the aneurysm will ideally shrink.
Great. So we're getting questions from our viewers. I want to get to as many as these as we possibly can. One that just came in is, can you explain the kind of pain that would be in your stomach? So again, it gets back to the symptoms.
Do you want to do-- no, I'm just joking. I'll do that.
I know, absolutely.
So the type of pain, the way I tell my patients, a lot of people we meet actually have chronic back pain. And sometimes an aneurysm gets discovered because someone has chronic back pain and that's getting evaluated. It is the worst pain you have ever felt in your life. It is excruciating pain. Whether it's back pain or abdominal pain, if you have pain that is not going away and is really severe pain, you need to be seen right away. Even if you don't know you have an aneurysm, if you have that type of pain, you need to be evaluated as soon as possible.
That's important. A couple more questions. When do you stent? This one is asking us, my husband has a 4.9 aneurysm and my doctor says to keep watching. I'm not sure exactly what they're referring to. I'm guessing that's the size, is that correct?
Yes. So typically-- and I don't want to make a generalization, that would be unfair just based on one question-- but the typical recommendations are when an aneurysm reaches about 5.5 centimeters in size, then when we look at the risk of the operation versus the risk of the aneurysm is when we say, this is time to repair. So typically a 4.9 we would say it's safe to watch. But that would be an individual decision that's made between each doctor and their patient.
And I have repaired some aneurysms at that size, and I was concerned with the patient or their risk factors or their symptoms. So I don't want to make a broad sweeping statement. But typically 5.5 centimeters, because that's where the risk of the aneurysm starts to outweigh the risk of the operation, and we say, yes, go ahead.
How risky is the operation?
So the operation, especially now with the stent approach to the groins, is very low risk. Any invasive procedure has some risk. The overall risk in terms of getting out of the hospital or having bad problems is exceptionally low, and certainly much lower than it was in the year when we did all open surgery.
Yeah, there's one part though is getting an aneurysm fixed, whether you're a man or a woman, makes a difference. Because we women tend to have smaller options. And so really good questions the patients should be asking is, how comfortable are you having an aneurysm? Do you want to get it fixed? And I know over the years that I've done this that peace of mind is a big deal too. But that's where you really have to work with your health care professional and make sure that you've chosen the one that you're comfortable with. And do your research, right?
Yes, absolutely.
And Jim, you've been tested. You mentioned your brother was tested and saved. All your family members-- have they been?
Every one of my family members has been made aware of to get screened. Now I can honestly say I don't know if everybody has. But it was really interesting with my brother Don is that when I worked for Gore, the blessing that I got back was this knowledge on how to take care and look for symptoms. And not only have I had my brother Don screen, but multiple friends that you just now know look like they should be done. And you ask different questions, and they're more prepared when they go in and get a physical, and there's a certain age where this is an important part of that.
But when we first tested my brother Don, he didn't have an aneurysm, but he needed open heart surgery. And then years later he had tests for an aneurysm, and he had one, and they did monitor it. They did take it out when it was time to have to take it out. And now happy to say is that his life has been saved through the hard work and awareness that we've all worked so hard to have like today.
Another question from a viewer. Their father died of an abdominal aortic aneurysm. He was a lifelong smoker. I'm a non-smoker. Is my risk of an aortic problem any higher because of his history? Or is this primarily caused by smoking?
Yeah. So aneurysms definitely run in families. It's not directly inherited. Just because Jim's dad had one obviously doesn't mean he's going to have one. And clearly he's been checked and does not. But there is a higher risk in families. And in fact, one of the things I've done with my patients now. And I think partly because of getting to know Jim like I have, is I tell all of my patients, yes, I will get you taken care of, but you need to tell your family members they need to get checked. Whether it's siblings, whether it's their children, I tell them when their children reach 50 they should have an ultrasound at age 50. And if it's fine, they don't have to be checked for 10 years. But if you have a family member-- especially a woman in your family that's had an aneurysm-- you should be checked, even if you don't have the other risk factors, because the family history alone is enough of a risk factor.
Now this is an interesting question from a viewer. Another viewer whose father died of this. And again, they don't smoke, but they also want to know what steps they could take to potentially prevent that. Are there steps you can take?
Yeah. So aneurysms, unfortunately, once they occur they're hard to prevent. Now the way to potentially prevent them from happening is-- you can't change your parents. You can not smoke and you can have your blood pressure well controlled and have your cholesterol well controlled. And that's really the most thing you can do to prevent an aneurysm from forming. But the risk that comes just from genetics obviously does not go away. But the biggest modifiable risk factors are smoking, blood pressure control, and cholesterol control.
So you mentioned screening 10 years. Oh, go ahead, I'm sorry.
One thing that I would like to that is these viewers are saying that their father died of it. But did their father have any siblings? Did anybody else in their family? Have they been able to be aware? Are they going to, after this show, go back and tell everybody that they know that's inside the family tree of what they're learning? Because that's really how you help make people aware.
And it's a quick test too.
Great point. Jim's making a great point. And it is an easy test.
The option is not good, folks. When they detect one and they're aware of it, the procedure and getting in and out is like a 98% success rate. But we don't you want to tell you what the success rate is when there's a rupture.
Well Jim, you even mentioned before the program, we were chatting and you said, people think about the cost of a test or that sort of thing. And you made a good point. And if you would make it to our viewers, that'd be great.
Yeah. I use the example. It's like the cost of a good bottle of wine. Why would you risk your life because you didn't get a free screening? If you at risk, you go in and be proactive when you meet with your primary care physician. If you're going to go get a physical and you're over 50 years old and you have any questions, you be the one to ask them and hold them accountable to be able to help you. Check in with your community and find out what kind of screening that's available. There's always screenings available through the churches or different organizations that you can help. And if not, be proactive and get one started.
And Dr. Milner, is this something that's covered by insurance? This type of screening.
So in the Ultimate SAAVE Act that is covered by Medicare is an introduction to Medicare when you have the appropriate risk factors. Otherwise it's not something that is typically covered. But as Jim, said number one, there are a lot of places that offer free screening. But number two, it's not a very expensive test that could be a lifesaving test. So from my perspective it's worth the cost. But as a Medicare introduction, you can get that when you have appropriate risk factors.
And so you suggest to folks at the age of 50, if they have risk factors, and then 10 years later. Is it then every decade? Or how does--
So if you don't have an aneurysm at 50 and at age 60, the likelihood of you developing an aneurysm later is very low. But again, because there's no risk to the ultrasound, I would say check every 10 years. You get to 70 and you're fine, then you can make a decision if you want to do it at 80. But we take care of patients commonly in their 80s and 90s with aneurysms that are good risk, that are healthy and still active and want to do things. And it's worth being checked.
Well, one of the things that was most amazing to me in working with Gore is that when I went around, and you saw in the old days when you had a vascular surgeon that didn't do anything but open, and they were uncomfortable with this endovascular repair. Then they would say to their patients, you're 80 years old, you're OK. But now these young doctors have such competence, and the product is so good that they're taking care of people at 92, 93, and they've got incredible quality of life. So don't let anybody tell you that you can't get this fixed because of age, because you can, and you should. And just make sure that you'd go out and you go to the right places as you guys were able to do a little brag about today, because you've earned it, right?
Yeah, thanks.
One of the things that I always like to talk about on the program is-- there's a couple of things-- and one of them is the team approach that we have, and you mentioned that earlier. It's so important to what we do. But the other thing that I think is a tremendous strength of this institution is the fact that it is a research institution. And so let's talk a little bit about our clinical trials research, what kind of things are going on here that might-- or anywhere-- that might impact this situation.
Yeah. So thanks for bringing that up, because I think one of the nice parts about working at a place like this is it is a teaching institution. And as part of that we do a lot of research. We do a fair bit a number of clinical trials. I'm involved on a national level in leadership roles with several clinical trials. And locally we're involved in multiple clinical trials here to look at devices as well. We do a lot of research, and we publish.
And in fact, one of the points that Jim brought up earlier was about screening in women. And we have a paper that we published here within the past few months in one of our prominent journals showing that in a ruptured aneurysm population study that was done that there was a much higher percentage of women that were expected. And that maybe when we do the screening we've looked for factors to screen, but maybe we haven't looked for all of them. So it's the really fun part, I think, of what we do in addition to the patient care is the academic part of what we do in a place like this. And I think we're trying to do it pretty well.
And why I was so excited about coming here is when I met Dr. Milner I compared him to a coach. Some coaches are really good at prepare for a game, and some coaches are really good when the game goes on. But very few of them are good at preparing and at the game. And so his love for being an advocate for medicine is just so obvious. And he's a great mentor, a teacher to the young.
But he stays very young at his profession, which is really great. And he forces change to happen within in the hospital, and it continues to get better. And it's just a pleasure to be able to be with you and learn, because that gives me an opportunity that when I go out with Gore to help and be more aware and more professional in the approach.
Thanks, Jim.
So I am curious, we've talked a lot about how much this impacts men, and you mentioned women as well. And there was one case that you talked about before-- and we won't get into specifics obviously-- but it is important for women to be aware of this as well. But their symptoms may be a little different. Is that correct?
Well, I think part of the problem is because it's such a predominantly male disease that even though maybe the symptoms aren't different in women, once again like Jim mentioned earlier, people just aren't thinking about it as commonly as they should. So the symptoms actually are not dramatically different, but the awareness for it is significantly different because everybody thinks, oh, it's an abdominal aneurysm. It's only men that have this disease. And that's not true.
And you don't want to go to an emergency room and get stuck when people aren't aware of what could be happening. And so that's really important to go to the right hospital and know that the people that are there-- the professionals that are there-- certainly know the risk factors and move a lot quicker than if you don't go to the right place.
Well, there we go. We're out of time.
That was so much fun.
It went quickly, didn't it?
Yes it does.
That is all the time we have on the program. Thank you for being on the show. We really appreciate it.
Thank you for having us.
Yeah, I think it's great.
I just think this is a cutting edge thing that we should think more of, and we will definitely get it out to the right people.
Perfect, perfect.
I think we covered a nice spectrum too, which is nice.
Absolutely. If you want more information, please visit our website site at UChicagoMedicine.org, or even call 888-824-0200. Also remember to keep an eye on our Facebook page for more events and live programs. We got another one coming up at the end of this week. Thanks for watching hope you have a great week.
Comer Children's Hospital at the University of Chicago Medicine is at the forefront of kids health, shaping national standards of care from infants to young adults. Comer Children's, welcome to the forefront.
This was a paid program from UChicago Medicine.
Other Conditions We Treat

Nationally Ranked in Cardiology, Heart Surgery and Vascular Surgery
According to U.S. News & World Report's 2025-26 Rankings

High Performing in Aortic Valve Surgery
According to U.S. News & World Report's 2025-26 Rankings
Nationally Ranked in Cardiology, Heart Surgery and Vascular Surgery

Find an Aortic Disease Specialist Near You
Request an Appointment
We are currently experiencing a high volume of inquiries, leading to delayed response times. For faster assistance, please call 1-773-702-6128 to schedule your appointment.
If you have symptoms of an urgent nature, please call your doctor or go to the emergency room immediately.
* Indicates required field