Coronary Artery Disease and Chest Pain
What is coronary artery disease?
The University of Chicago Medicine is home to expert heart specialists that excel in the diagnosis and treatment of coronary artery disease.
At UChicago Medicine, our cardiologists and heart surgeons have unparalleled experience treating patients with complex diseases or those with co-existing medical problems, such as diabetes. We also consistently take on the most challenging cases – even those considered untreatable.
Our expert cardiac surgeons are highly skilled in minimally invasive coronary artery bypass surgery and perform various procedures through small incisions rather than cracking open the chest. Benefits of these approaches include a faster recovery, less risk for complications and less pain compared to traditional open-chest bypass surgery.
Symptoms and Risks of Coronary Artery Disease
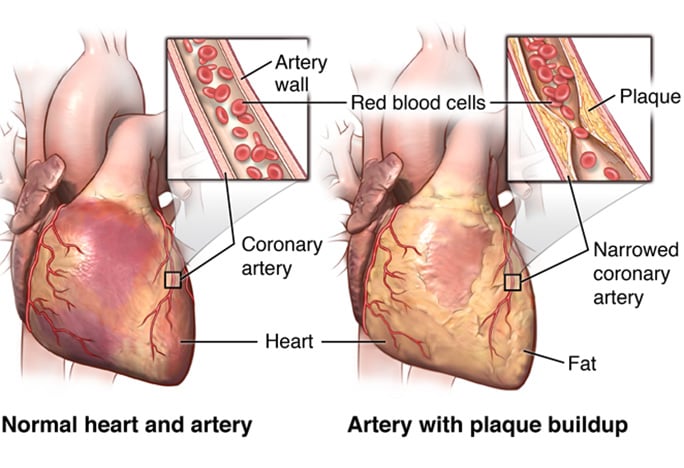
As the leading cause of death in Americans, coronary artery disease is a serious condition, and when it is allowed to progress, it can be fatal. Unfortunately, it can be difficult to know if you are in danger because while coronary artery disease is caused by a build up of plaque on coronary arteries, it is often not apparent that you have heart disease. As the plaque continues to accumulate, the arteries will narrow, eventually slowing or even blocking blood flow throughout the body. To prevent serious complications, it is critical to know the common risks for coronary artery disease in order to identify an issue and seek treatment before the disease becomes unmanageable.
Coronary Artery Disease Causes and Risk Factors
Coronary artery disease is thought to begin with damage or injury to the inner layer of a coronary artery. The damage may be caused by various factors, including:
- Age
- Diabetes
- Family history of coronary artery disease
- High blood pressure
- High cholesterol
- Low mobility
- Obesity
- Smoking
Coronary Artery Disease Symptoms
If you are at risk because of one or more of the above conditions, do not ignore complications that can cause or exacerbate coronary artery disease. If you have or experience any of the following conditions, reach out to your doctor as soon as possible:
- Chest pain (angina)
- Heart attack (pain in the arm, jaw, lightheartedness)
- Shortness of breath
Chest Pain: Frequently Answered Questions
Chest pain is a key symptom of coronary heart disease, which the most common type of heart disease that kills 370,000 people annually. Because we know that it can be hard to identify when chest pain could be a warning sign of heart disease, our heart experts answered some common questions about chest pain to help explain when it could be serious.
Chest pain can be caused by many things, and while chest pain can be because of gas or indigestion, it could also be a sign of heart disease. It is important to think about the type of chest pain you are having to help identify the severity and/or progression of the chest pain:
- Is the pain is causing exertion and worsening?
- Does the chest pain take your breath away, make your nauseous?or
- Has it even made you pass out previously?
These are serious clues that there could be a more serious cause of your chest pain.
Because chest pain can be a something that requires medical attention, even if your chest pain gets better with rest, bringing this to your doctor’s attention is always a good step to catching heart disease early.
Risk factors like smoking, high blood pressure, diabetes, a strong family history of heart disease and/or a personal history of high cholesterol should be considered when you experience “heartburn.” If you have one or a combination of those risks, in addition to any chest pain symptoms, you should not ignore them.
If your heartburn/chest pain gets worse, particularly if it worsens when you walk around, it's probably not heartburn and is more likely related to your heart. Because your heart needs energy to perform, it demands more energy when you exercise. Whenever chest pain symptoms get worse when you walk around, it could be due to the lack of blood flow to your heart when you're walking around.
Generally speaking, sharp pains that are fleeting and feel like electric shocks or pinpricks are less likely to be related to heart disease. But that's a very broad statement and we recommend you meet with your doctor to fully understand the pain you are experiencing.
Start with an assessment of your cardiovascular risks. This usually includes bloodwork, blood pressure screen, perhaps an electrocardiogram (ECG), and some lab tests to get a better sense how high your risk for heart disease is. Based on this information, we can recommend more in-depth tests and develop a comprehensive treatment plan.
A calcium CT scan is a very easy, inexpensive way to figure out your cardiovascular risks. Early detection is vital to prevent its progression and reduce the risk of heart attacks and strokes. A calcium CT scan allows us to:
- Identify Early Signs: Even before symptoms appear, a calcium CT scan can detect the presence of calcified plaque in your arteries.
- Assess Risk Accurately: By calculating a calcium score, we can determine your risk level for heart disease more precisely.
- Guide Preventative Care: With the information from your scan, our healthcare providers can develop a personalized prevention plan tailored to your specific needs.
Don’t wait for symptoms to take action. A calcium CT scan is a proactive step towards ensuring a healthy heart. If you have risk factors such as a family history of heart disease, high cholesterol, high blood pressure, or are a smoker, consider scheduling a calcium CT scan with us.
Find a Chest Pain and Coronary Artery Disease Location Near You
Request an Appointment
We are currently experiencing a high volume of inquiries, leading to delayed response times. For faster assistance, please call 1-773-702-9461 to schedule your appointment.
If you have symptoms of an urgent nature, please call your doctor or go to the emergency room immediately.
* Indicates required field
