Are you at risk for fatty liver disease?

Fatty liver disease (steatotic liver disease) affects up to one in three American adults. At the University of Chicago Medicine Steatotic Liver Disease Clinic, my colleagues and I work across disciplines to treat patients with this common disease, which can lead to liver failure and the need for a liver transplant.
Request an appointment for fatty liver disease evaluation.
Here are answers to frequently asked questions about the increase in fatty liver disease, what patients can do to lower their risk factor and when they should talk to their doctors about getting assessed.
What is fatty liver disease?
Fatty liver disease, or steatotic liver disease, is the term for a range of conditions in which excess fat is stored in the liver cells of people who drink little to no alcohol. Alcohol also causes fat to accumulate in the liver, and even lesser amounts can compound the risk of liver damage in someone with steatotic liver disease.
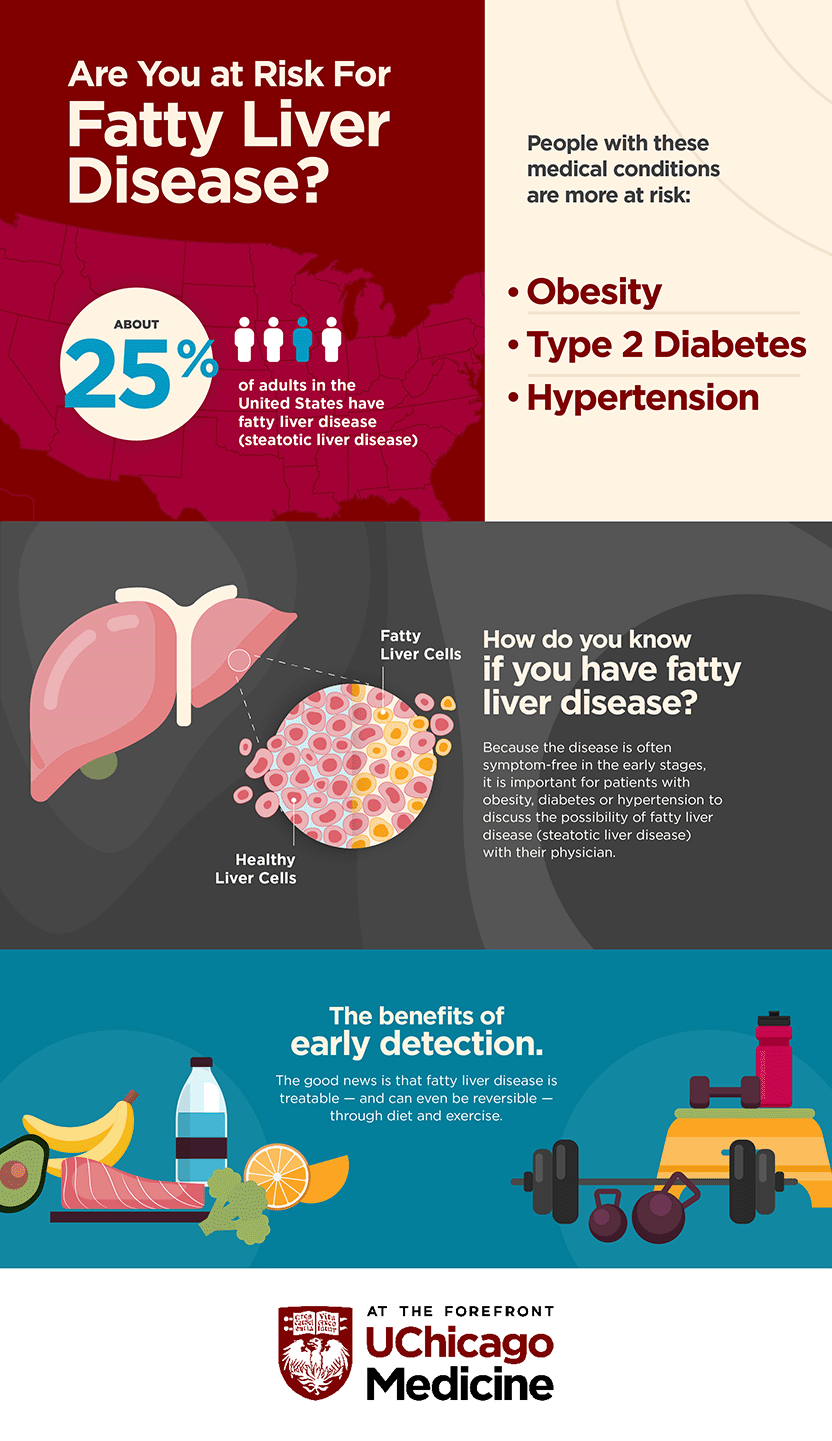
The disease is increasingly common in Western nations, and the majority of people with fatty liver disease also have other associated medical conditions, notably obesity, type 2 diabetes and hypertension.
It is important for patients with obesity, diabetes or hypertension to discuss the possibility of fatty liver disease with their physician.
Because the disease is often symptom-free in the early stages, many people do not know they have it. But some patients who have fatty liver disease can go on to develop nonalcoholic steatohepatitis (NASH), a more aggressive form of fatty liver disease associated with increased liver damage, inflammation and scarring that can progress to cirrhosis and liver failure.
What causes fatty liver disease?
Both obesity and type 2 diabetes favor the development of fatty liver disease. That’s because overnutrition and insulin resistance result in excessive delivery of fatty acids into the liver. This leads to the accumulation of fat in the liver as the delivery of fat exceeds the liver’s ability to utilize it or export it.
Can certain foods cause fatty liver?
Certain foods are more likely to promote the development of fatty liver, such as those rich in carbohydrates and saturated fat. Concentrated fructose, common in many processed foods, is particularly damaging because it is converted into fat in the liver, without impacting satiety.
Who is most at risk for fatty liver disease?
Obesity and type 2 diabetes are increasing steadily in the United States. More than 40% of adults are now considered obese, and more than 10% of the U.S. population has diabetes, the majority of which is type 2 diabetes. That means that more people are at risk for steatotic liver disease. Diabetics also are much more likely to develop the severe forms of fatty liver, such as NASH and cirrhosis, than non-diabetic patients.
How do you know if you have fatty liver disease?
Most of the time, steatotic liver disease doesn’t produce any symptoms. That’s why it is important for patients with risk factors such as obesity, diabetes or hypertension to discuss the possibility of fatty liver with their physician. While the majority of people with fatty liver don’t go on to develop cirrhosis, it has become the most common reason for liver transplants in women and individuals over 65 years of age. With increased awareness and early detection, those at high risk for developing liver cancer and liver failure can be diagnosed and treated in time.
What diseases are connected with fatty liver disease?
In addition to obesity and type 2 diabetes, hypertension also is associated with fatty liver disease, and has been tied to more progressive forms of the disease. Right now, about 25% of adults in the United States have fatty liver disease, and about 25% of those individuals will have NASH. But within the diabetic population, 75% have fatty liver disease and 50% of them have NASH.
Alcohol use clearly causes fat to accumulate in the liver. Some studies have shown that regular marijuana use can increase fat accumulation in the liver and worsen scarring, but more research needs to be done.
What tests are used to diagnose fatty liver?
One of the simplest ways to understand the risk is to do a calculation called Fibrosis-4 (FIB-4). The scoring system is based on liver enzymes, platelet counts and a patient’s age. Using those parameters alone, you can reassure the majority of people that they don’t have high risk for severe liver disease. Those who are considered more at risk should have their liver stiffness assessed with a FibroScan, available mostly in GI/hepatology practices, or through specialized ultrasound or MRI techniques. Since liver stiffness is often related to scarring, this noninvasive procedure helps your doctor to exclude the possibility of severe scarring or identify the need for further evaluation.
At what age do people get fatty liver disease? When should people be tested for it?
The longer your body is exposed to excess abdominal weight, the more time for fat to accumulate in your liver, and the more likely scarring will accumulate. Therefore, we do see a worsening of fatty liver disease severity in patients as they age. It may take 30 years for fatty liver to turn into cirrhosis (unless the patient has a genetic predisposition), so the typical age people are diagnosed with cirrhosis is 60.
That said, people are becoming obese at a younger age now. So, those who have been obese their whole lives are at risk in their 30s, or in some cases earlier. Cirrhosis from fatty liver is even seen in some adolescents. Studies show that by 2030, the risk for liver-related cancer will increase by 168% and the risk of cirrhosis and pre-cirrhosis will go up by 178%. We’re going to see not just a lot more people with this disease, but a lot more people who become sick from it.
What do should you do if you are told you have fatty liver? How is the disease treated?
The core principles of treatment are nutrition and lifestyle interventions, especially at the early stages of disease when disease progression can be prevented. Steatotic liver disease is most importantly impacted by weight loss and physical activity. If you just have a fatty liver with no inflammation or scarring, the fat can be reduced in a matter of weeks to months through diet and exercise. To be successful in improving liver disease, weight loss needs to be sustained. This is why it's so important to have ongoing support from a nutrition expert with expertise in treating fatty liver, as we have in the UChicago Medicine Steatotic Liver Disease Clinic. Beyond that, some drugs that treat obesity and diabetes may be beneficial in fatty liver disease.
If a patient already has inflammation and scarring, it is harder to treat, but not impossible. In patients who lose 10% of their body weight, scarring has been shown to improve, and it becomes extremely unlikely that their disease will progress. Patients who already have scarring should also not drink alcohol, since a safe level of alcohol intake is unknown for people with fatty liver disease.
What happens if fatty liver goes untreated? Can you live a long life?
For those with a low FIB-4 score, it is unlikely that the disease will progress to severe stages. Many people who have fat in their liver never die a liver-related death, but fatty liver does increase your risk for other diseases, including type 2 diabetes, hypertension, heart disease and cancer. In fact, a disproportionate number of people with fatty liver disease will die from heart disease or cancer. And those who have fatty liver disease that progresses ultimately could need a transplant or develop liver cancer, which could lead to complications and even death.

Mary E. Rinella, MD
Dr. Rinella is an expert in fatty liver disease (steatotic liver disease). She provides comprehensive liver disease assessment and treatment, including nutritional intervention, the use of medications, endoscopy and clinical trials to deliver the most advanced treatment options.
See Dr. Rinella's physician bio