New technology lets UChicago Medicine safely transport donor lungs from across the US

It was hard for Herbert Dresbaugh, Jr., to accept that he’d need a lung transplant one day.
The 69 year old had been so healthy his whole life; he'd never once needed prescription medication. But in 2016, he was diagnosed with severe idiopathic pulmonary fibrosis, a disease his father had, which progressively scars the lung tissue and makes it increasingly difficult to breathe. Within a few years, his health deteriorated.
“He was huffing and puffing just putting his shoes on, and that was while using oxygen,” said his daughter, Dawn Peterson, a nurse. “His doctor said it’s time to ‘list him’ for a lung transplant. We just prayed and waited. He didn’t have much time left.”

Within weeks, the transplant team at the University of Chicago Medicine found Dresbaugh a perfect set of donor lungs — in Texas, more than 1,200 miles away. Traditionally, transplanted lungs can only come from donors within 500 miles of a patient who needs the new organs. That's because the organs' lung function begins to deteriorate after six hours. Recovering donor lungs in Texas, preserving them on ice, flying them to Chicago, and then performing the transplant would take too long.
Not anymore. In May 2019, UChicago Medicine started using the TransMedics OCS Lung (OCS stands for organ care system). This state-of-the-art device keeps donor lungs viable more than three times longer than other methods, allowing the transplant team to choose from donors from all over the country, improving the quality of lungs the patients’ receive and shortening their wait time for a transplant. UChicago Medicine is the only hospital in Illinois to offer this groundbreaking and life-saving technology for lung transplantation.
This state-of-the-art device keeps donor lungs viable more than three times longer than other methods, allowing the transplant team to choose from donors from all over the country.
It allowed Dresbaugh to receive the lungs from Texas, have a successful transplant surgery in the summer of 2019, and return to his normal life running his family’s automotive machine shop business in Lake Village, Indiana.
TransMedics OCS Lung is the only FDA-approved, portable Ex Vivo Lung Perfusion (EVLP) device that supports recovered donor lungs by keeping them warm rather than cold. The device circulates oxygenated blood through the lungs for up to 20 hours, allowing them to travel 1,500 miles or more safely. Already, there’s been Tae H. Song, MD, UChicago Medicine’s Surgical Director of the Lung Transplant Program. That’s because EVLP allows the team to monitor and recondition the lungs, ensuring they’re in the best possible condition for the patients.
“We have the opportunity to optimize the lungs before they’re transplanted,” Song said. “We’re accepting donations from far away on a routine basis now.”
The user-friendly technology adds an extra layer of comfort for both doctors and patients, added David Onsager, MD, the UChicago Medicine surgeon who does most of the hospital’s lung procurements.
“When there’s an urgent need for a transplant, you’re better off taking a not-exactly-perfect set that you can tune up on the machine, as opposed to waiting several more weeks searching for a perfect donor,” he said. “Now we get to see the donor lungs working well before we proceed.”
UChicago Medicine has used TransMedics OCS Lung for 17 successful lung transplants in the past 18 months. In January 2021, UChicago Medicine’s transplant team used it for two lung transplants within 24 hours. They also used it for a transplant on a patient whose lungs were damaged by COVID-19.
It also gives UChicago Medicine surgeons the ability to do multiple transplants in short succession. This is because lungs can remain on the TransMedics OCS Lung device for an extended period of time while other transplants are occurring.
The technology has been so encouraging, UChicago Medicine could begin using similar systems for other donor organs in the future. The hospital already participated in the clinical trial for TransMedics OCS Heart, a similar organ care system for donor hearts.
UChicago Medicine has emerged as one of the country’s leading transplant programs, known worldwide for its willingness to take on some of the most complicated cases.
UChicago Medicine has emerged as one of the country’s leading transplant programs, known worldwide for its willingness to take on some of the most complicated cases. Demand for lung transplants is expected to increase, given that COVID-19 can potentially cause long-term damage to the lungs, Song said.
“This technology is going to be a key part of lung transplantation in the future,” he said.
Song performed Dresbaugh’s transplant surgery, which went so smoothly, Dresbaugh was out of the hospital in nine days. Within two weeks, he was able to return to work a few hours a day. Now 72, Dresbaugh says his life is back to normal. His daughter says he’s more energetic now than before his transplant.
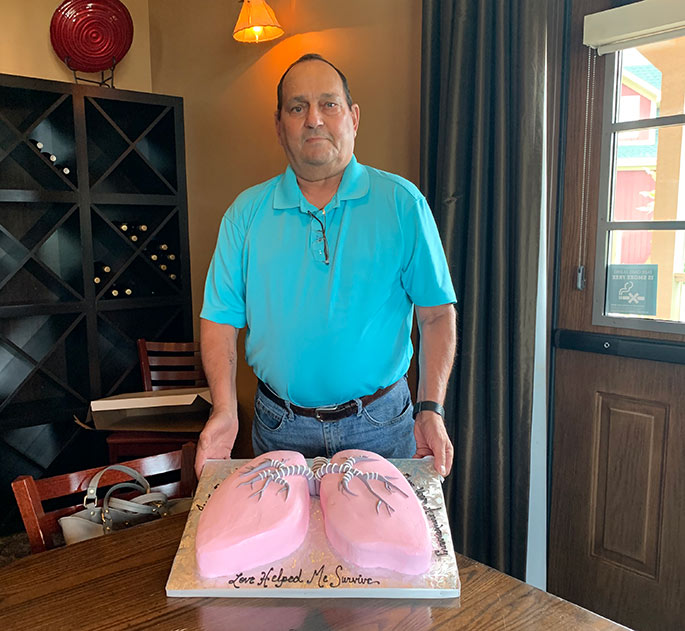
“I feel fantastic,” Dresbaugh said in January 2021. “I don’t have trouble breathing, and I haven’t had to use oxygen again. A friend of mine who also needed a lung transplant for the same disease saw how well I was doing, so he went for evaluations and was able to have a lung transplant at UChicago Medicine about 4 ½ months later. He’s doing phenomenally well, too.”
Lung Transplantation at UChicago Medicine
Whether you have a straightforward condition or a very complex case, our lung transplant specialists have the expertise to help you. We treat a variety of lung conditions, including cystic fibrosis, pulmonary hypertension, Alpha-1 antitrypsin deficiency and pulmonary fibrosis.
Read more about our lung transplant program
David Onsager, MD
David Onsager, MD, is a highly skilled thoracic surgeon. Dr. Onsager has expertise in heart and lung transplantation.
See Dr. Onsager's physician profile