Stem cell-derived components may treat underlying causes of PCOS
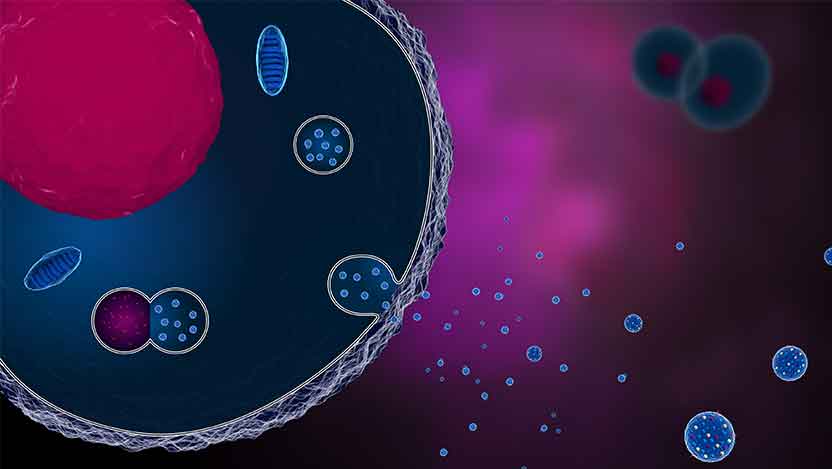
Extracellular vesicles (EVs) are tiny packages released by cells as a means of communication with other cells. In the context of treating PCOS, EVs derived from mesenchymal stem cells (MSCs) have shown therapeutic potential due to their ability to produce factors that can regulate cell behavior and reduce inflammation.
Polycystic ovary syndrome (PCOS) is a pervasive endocrine disorder that affects millions of women globally, impacting their hormonal balance, fertility and overall well-being. It is notoriously difficult to treat, with widely varying symptoms and mysterious, complex underlying causes. Recently published results demonstrate the promise of this novel therapeutic approach that uses mesenchymal stem cell-derived extracellular vesicles (EVs), also known as exosomes: tiny, free-floating packages of molecules released by stem cells.
“Current PCOS treatments merely address the symptoms, and the most common treatments – oral contraceptives – do not address patients’ struggles with infertility,” said Hang-Soo Park, PhD, staff scientist at UChicago and the study’s first author. “Our approach represents a paradigm shift from symptom management to treating the underlying causes. We hope this will prove more effective in the long term and allow patients to have children if they wish to do so.”
The group had previously published findings that mesenchymal stem cells (MSCs) – adult cells that can differentiate into multiple cell types for healing and regeneration – can secrete factors that can help reverse the symptoms of PCOS, but it was unclear what those factors were. The latest study identifies the EVs they release as the therapeutic components.
The researchers found that MSC-derived EVs lowered the activity of genes that contribute to the overproduction of androgen hormones — a hallmark of PCOS. Based on this finding, the scientists injected the EVs into mouse models of PCOS, where they helped stabilize some of the metabolic irregularities often associated with the disorder, such as high glucose levels. The EVs can be injected into either blood vessels or directly into the mice's ovaries, and in both cases, they actually restored ovarian function.
“Our study demonstrates the resilience of the ovaries under EV treatment, offering renewed hope for women battling PCOS-related fertility issues,” said Park.
The researchers believe an immune signaling protein called IL-10, known for its anti-inflammatory properties, may play a key role in the healing they observed. The EVs may serve as delivery vehicles that stabilize IL-10 and ferry it to target cells, increasing the molecule's effectiveness in reducing inflammation and driving restorative processes.
EV-based therapy showcases distinct advantages over conventional methods. Unlike whole stem cell therapy, EVs are more accessible and less expensive to use, making them well-suited for wide-scale applications. They also offer a better safety profile, with minimal concerns about tumorigenesis or immunogenicity. Notably, clinical trials using EV therapy for reproductive disorders have already garnered approval, demonstrating the high potential for translating this research into real-world benefits.
Park pointed out that some companies are already commercially manufacturing EVs that have proven safe in clinical trials. As a result, he said producing a therapeutic will not be technically challenging once the design is finalized.
Park is now applying for grants to fund human clinical studies of this EV treatment. Simultaneously, they are performing additional bench research with the goal of developing enhanced EVs that more precisely target ovarian tissue, potentially reversing damage more effectively.
“The key takeaway for PCOS patients right now is that researchers are working hard to understand the pathways involved,” said Park. “As we understand more and more, the treatments will become even safer and more effective.”
The study, “Therapeutic Potential of Mesenchymal Stem Cell-Derived Extracellular Vesicles to Treat PCOS,” was published in the International Journal of Molecular Sciences in July 2023. Co-authors include Esra Cetin, Hiba Siblini, Jin Seok, Hiba Alkelani, Samar Alkhrait, Farzana Liakath Ali, Mohammad Mousaei Ghasroldasht and Analea Beckman.
