New drug shows promise for improving islet transplant outcomes in some type 1 diabetes patients
Preliminary results from an ongoing clinical trial at the University of Chicago Medicine suggest that a new drug aimed at preventing the rejection of transplanted islet cells may improve outcomes for a small number of patients with 'brittle' type 1 diabetes who struggle with especially unstable blood sugar levels.
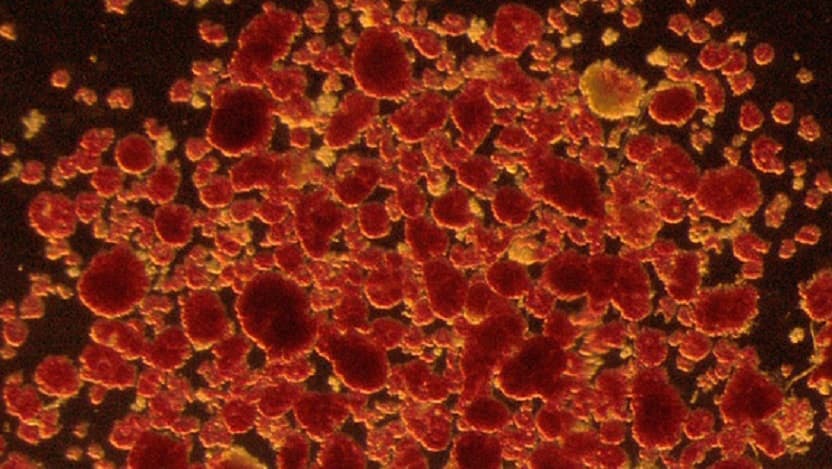
Islet transplantation involves infusing donor islets – insulin-producing cells taken from a healthy pancreas – into a diabetic patient's liver via a minimally invasive procedure. Once successfully transplanted, these cells start producing insulin to help regulate blood sugar levels naturally. The treatment remains an experimental procedure in the U.S., and UChicago Medicine is one of just a few centers offering this therapy through clinical trials.
Traditional immunosuppressive drugs used to combat transplant rejection can damage islet cells, necessitating multiple transplant procedures and potentially causing significant side effects like kidney damage, increased risk of hypertension, or even new-onset diabetes. “We’ve spent decades seeking alternatives that will prevent rejection without these adverse effects,” said Piotr Witkowski, MD, PhD, director of the pancreatic and islet transplant program at UChicago Medicine.
In the recent trial, three patients with type 1 diabetes received islet transplants along with the investigational antibody drug tegoprubart to prevent transplant rejection. Two participants achieved normal, stable blood sugar levels, completely freed from the need for insulin injections, while the third participant reduced insulin use by more than 60% within days of the transplant and, as of this article, remains on track to stop insulin use in the future. Overall, researchers estimated that islet engraftment in patients treated with tegoprubart was three to five times higher than in those receiving standard immunosuppression drugs, and no unexpected adverse events were reported.
"Our hope is that these findings will eventually pave the way for wider adoption of islet transplantation as a standard therapy for brittle type 1 diabetes," Witkowski said. "At UChicago Medicine, we already have five transplant recipients who have been enjoying life without insulin for over 10 years. If we successfully validate an immunosuppressive regimen that is both safe and effective, it will allow more patients to benefit from this potentially life-changing procedure in the future."

Piotr Witkowski, MD, PhD
Dr. Witkowski is a leading expert in islet transplantation. He was instrumental in developing an optimized islet isolation technique that greatly improved success in clinical transplants.
Learn more about Dr. Witkowski