Tiny valves help some emphysema patients breathe better – and avoid surgery
Bronchoscopic lung volume reduction is a new, reversible procedure that involves no surgery and can help patients with severe emphysema breathe better.
Even though we take tens of thousands of breaths every day, this critical inborn ability is something we rarely ever think about until we face a health problem that impacts our lungs.
For the 3.8 million Americans diagnosed with emphysema, every cough, wheeze and shortened breath is a reminder of the impact of this devastating disease. Emphysema is a type of chronic obstructive pulmonary disease (COPD) in which tiny air sacs in the lungs called alveoli narrow, collapse or are otherwise damaged. This damage is most often caused by smoking, although air pollution, chemical fumes, dust and a rare genetic mutation called Alpha-1 antitrypsin deficiency can also cause it.
People with emphysema have difficulty breathing, so patients are treated with bronchodilators (medicines that reduce swelling) and inhaled steroids to help widen the airways of the lungs. Patients with severe emphysema often receive extra oxygen through a slender tube connected to a portable oxygen container.
These treatments do not, however, repair or regrow damaged lung tissue – and symptoms only worsen with time.
This simple treatment involving no pain can replace a complicated, risky surgery.
“A lot of people with emphysema end up with a region of the lung that’s very destroyed and a region that’s not so destroyed,” said pulmonologist D. Kyle Hogarth, MD, the medical director of the Pulmonary Rehabilitation Program and the Director of Interventional Bronchoscopy at the University of Chicago Medicine.
Not only does this destroyed part of the lung not work well, it also puts pressure on the remaining healthy lung. Air becomes trapped in the injured airways of the damaged lung, making it unable to deflate; this hampers the ability of the healthy lung to expand and contract as it works extra hard to take in oxygenated air and express carbon dioxide.
For patients with severe emphysema and for whom medications are no longer effective, treatment options have traditionally been limited to two types of major surgery: lung volume reduction surgery (LVRS) and lung transplantation.
Physicians began performing LVRS in the 1990s after experimentation with the procedure in the 1950s. The surgery involves cutting out damaged lung tissue; studies show patients with severe emphysema can breathe better afterwards. But LVRS is a complex, high-risk surgery: Surgical stitches in the lungs can leak air and cause serious complications, and patients undergoing LVRS have an increased risk for infections, stroke, bleeding and heart attack.
Patients who are not able to undergo LVRS may be able to receive a lung transplant. Transplant patients must take powerful anti-rejection medications for the remainder of their lives to make sure their bodies do not reject the new lung, and these medications can cause secondary health problems.
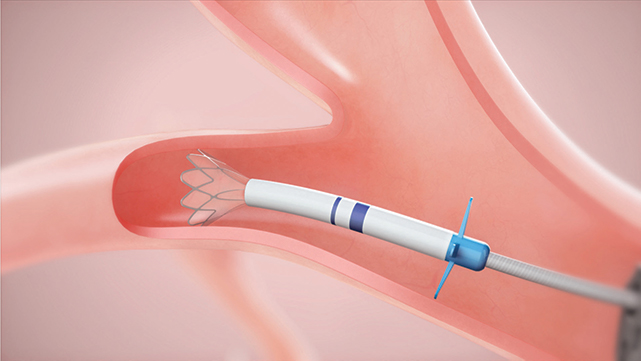
A new procedure using tiny one-way valves means patients who have little to no ventilation in damaged lung tissue may be able to avoid these risky surgeries altogether. The procedure is called bronchoscopic lung volume reduction (BLVR) and involves placing Zephyr endobronchial valves in specific airways to block off diseased parts of the lungs; these valves deflate the diseased lung so that air is no longer trapped inside and no new air can enter. Hogarth is a leading authority on the procedure in the United States.
“By having the lung collapse down in that targeted region, it’s similar to cutting out the tissue because it no longer takes up space,” said Hogarth. “So then the healthy part of the lung can expand and do more of the work.”
The valves can be inserted during a bronchoscopy, a procedure that involves inserting a thin, lighted tube through a patient’s mouth, down their windpipe and into their airways. Patients are given anesthesia, but no surgical cuts are involved.
“It’s a pretty straightforward procedure,” says Hogarth. “It’s actually wonderful in its simplicity though it’s clearly quite technical underneath. This simple treatment involving no pain can replace a complicated, risky surgery.”
The procedure usually takes 30 minutes, and clinical trials show that the valves successfully reduce shortness of breath while improving lung function, exercise capacity and quality of life. The valves are also removable, meaning the procedure can easily be undone if patients do not benefit from the treatment.
Breathing tests and a specialized CT scan at UChicago Medicine can determine whether patients are eligible for the procedure.
D. Kyle Hogarth, MD
D. Kyle Hogarth, MD, is an expert in pulmonary diseases — including lung cancer and alpha-1 antitrypsin (AAT) deficiency. He is an expert in the minimally invasive diagnosis, management and staging of lung cancer through bronchoscopy. He is a leader in advanced bronchoscopy using electromagnetic navigation systems that employ 3D imaging technology to detect and biopsy lung nodules and masses.
Read Dr. Hogarth's physician profile.