Movement disorders: What you need to know about diagnosis and treatments

Movement disorders are a group of nervous system (neurologic) conditions that affect a person’s ability to control their body movement. Parkinson’s disease, essential tremor, dystonia and tardive dyskinesia are examples of movement disorders.
At the University of Chicago Medicine, our multidisciplinary team of specialists treats the full range of movement disorders with the latest medications and surgical treatments, including deep brain stimulation (DBS). UChicago Medicine was the first hospital in the Chicagoland area to use the new Percept PC DBS system to treat patients with movement disorders.
What causes movement disorders?
We don’t know the exact cause of most nervous system disorders. In rare cases, dystonia and Parkinson’s are genetic. Essential tremor can be inherited, so if you have a family member with a tremor — and no other symptoms — there is a high likelihood you will develop the condition later in life. Tardive dyskinesia is caused by long-term use of anti-psychotic medications.
What are some early warning signs of movement disorders?
For Parkinson’s, one of the first symptoms can be a reduced, or loss of, sense of smell. This can occur as much as a decade before the movement disorder kicks in. Another early symptom is a sleep disorder. Focal dystonia often starts with muscle contractions in the neck, face or arms. Essential tremor usually begins gradually, with shaking hands.
While 0.5% of the population over the age of 45 develops Parkinson’s disease, we don’t yet know how to identify those who are at risk for the condition. Blood tests are being evaluated to detect early biomarkers of the disease and seem to be promising.
How are movement disorders diagnosed?
If you are concerned you may have a movement disorder, the first step is to see a neurologist to review your symptoms. Imaging of the brain and body may be performed to ensure the correct diagnosis.
What is deep brain stimulation?
Deep brain stimulation (DBS) uses electric impulses to regulate brain activity. It involves surgically implanting electrodes in the brain, which are connected to a pacemaker-like device placed under the skin near the collarbone. The electrical impulses essentially “silence” the hyperactive parts of the brain, lessening the symptoms of the movement disorder.
What is the new Percept PC DBS system?
The Percept PC DBS system not only stimulates the brain, but also takes recordings, allowing us to see how the brain responds to the stimulation. For example, if a patient experiences a symptom, such as a gait freeze, we can look back and see how their brain activity changed at that moment. Then we can tailor the stimulation specifically to the patient's symptoms and what they are experiencing.
How does this new system change how you treat movement disorders?
The Percept PC DBS system represents a new area of individualized treatment for our patients, and should provide more symptom relief. It also opens a lot of options to further research on movement disorders. For example, the scientific literature indicates that patients with young-onset Parkinson’s disease may benefit from undergoing DBS right away, instead of starting with medication. We are part of a phase 3 clinical trial, under which we will treat patients with DBS shortly after diagnosis. With the Percept system, we can understand exactly how this treatment affects the patient.
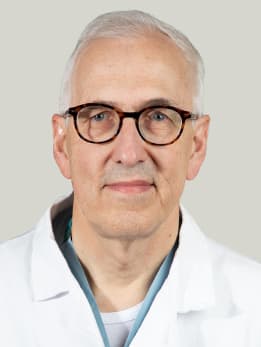
Peter Warnke, MD
Internationally renowned neurosurgeon Peter Warnke, MD, has performed more than 5,000 stereotactic surgeries and more than 2,000 brain tumor surgeries. Dr. Warnke provides neurosurgical care for the treatment of adults and children with movement disorders, epilepsy and brain tumors.
Learn more about Dr. Warnke