Expanding access to faster, cheaper radiation treatment for U.S. breast cancer patients
Hypofractionated whole-breast irradiation (HF-WBI) is a method of delivering radiation therapy after breast-conserving surgery. The treatment is highly efficient, less expensive, and takes less time; however, it is not currently the standard method of radiotherapy in the United States. Recent research from the University of Chicago Medicine Comprehensive Cancer Center examined challenges to more widespread adoption of HF-WBI, suggesting ways to address them so more women in the U.S. can benefit from this new treatment.
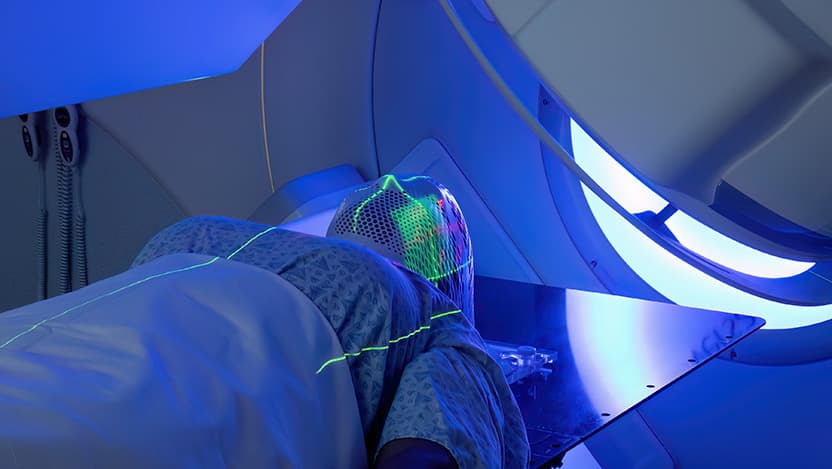
Radiation therapy for breast cancer is typically given after surgery. Traditional radiation treatment, known as conventional fractionated whole-breast irradiation (CF-WBI), delivers small doses of radiation in daily sessions spread over five to seven weeks. While effective, it requires a significant time commitment for patients and can lead to uncomfortable side effects like skin irritation and fatigue.
In contrast, HF-WBI delivers larger doses of radiation in each session, allowing the entire treatment to be completed in just three to four weeks. A shorter treatment course not only saves patients time, but also reduces the overall costs associated with cancer treatment, including transportation and time off work. HF-WBI also has fewer side effects and is just as effective as CF-WBI in preventing cancer recurrence. Together, these advantages make HF-WBI an attractive option for patients.
A team of researchers led by Loren Saulsberry, PhD, Assistant Professor of Public Health Sciences at UChicago Medicine, has conducted a series of studies to investigate trends in HF-WBI use and its costs. Their work is already building a greater understanding of barriers slowing its adoption in the U.S. While HF-WBI has been widely adopted in Canada and across Europe, its uptake in the U.S. has lagged. A 2022 study by Saulsberry and her colleagues showed that its use is increasing, however, and if trends continue, HF-WBI will soon become the dominant form of radiation treatment in the U.S.
That study also found that women from communities with higher levels of education and more racial diversity were more likely to receive HF-WBI, suggesting that socioeconomic disparities may affect access to such newer, innovative treatments. Where a patient lives also significantly impacts their chances of receiving HF-WBI. Certain regions, especially urban areas with more advanced medical facilities, are more likely to offer this treatment than rural ones, for example.
Follow-up research showed that doctors play an important role in the use of HF-WBI too, especially when they recommend treatment options to patients. In a study published in 2024, Saulsberry and her team found that the variation in HF-WBI use could be attributed mostly to differences at the physician level. In fee-for-service systems like the U.S., healthcare providers often receive higher reimbursements for longer treatments like CF-WBI because more sessions can be billed. While HF-WBI is more cost-effective, the overall economic structure of healthcare, particularly the way doctors are paid, may unintentionally favor the use of conventional, longer treatments.
Insurance also determines which treatments patients receive because it directly impacts out of pocket costs for patients. Since employer-sponsored private insurance is the dominant form of health coverage in the U.S., Saulsberry and colleagues evaluated the private insurance market. They wanted to explore variation in health insurance plan types and the cost differences across U.S. states in HF-WBI compared to CF-WBI. That study, the first of its kind, found no evidence indicating that a financial disincentive provided barriers to HF-WBI; however, even though private insurers cover the treatment, the authors suggested that healthcare policy reforms may be necessary to further promote its use. Just as doctors consider potential reimbursements when recommending treatments, insurers may have a strong incentive to encourage the use of HF-WBI due to its lower overall cost.
In the most recent study, Saulsberry and her team highlighted the growing preference for HF-WBI among people with Medicare Advantage (MA) health insurance, which are benefits provided through private insurance companies that contract with the federal government. Although there is considerable variation in the use and cost of MA across different regions of the U.S., the clinical and economic benefits have led to increased use of HF-WBI among these patients.
As more data emerges supporting the effectiveness of HF-WBI, studies like these will identify the drivers of HF-WBI use and the sources of variation in costs. As Saulsberry and her team learn more, they hope to help improve the quality of breast cancer care delivered to Americans by increasing access to this new form of radiation therapy.
Funding: National Institutes of Health
Citations:
- Hypofractionated Radiation Therapy for Breast Cancer: Financial Risk and Expenditures in the United States, 2008 to 2017. International Journal of Radiation Oncology, Biology, and Physics; 2022. Additional authors include Chuanhong Liao and Dezheng Huo from the University of Chicago.
- Geographic and Physician-Level Variation in the Use of Hypofractionated Radiation Therapy for Breast Cancer in the U.S.: A Cross-Classified Multilevel Analysis. Advances in Radiation Oncology; 2024. Additional authors include Yijia Sun, Chuanhong Liao, Donald Hedeker, and Dezheng Huo from the University of Chicago.
- Expenditures and Use of Hypofractionated Radiation Therapy Treating Breast Cancer Among Medicare Advantage Enrollees, 2009 to 2017. Advances in Radiation Oncology; 2024. Additional authors include Chuanhong Liao and Dezheng Huo from the University of Chicago.
