Could neutrophils be the secret to cancer’s Achilles’ heel?
A study published in the June 10, 2021 issue of Cell describes a remarkable new mechanism by which the body’s own immune system can eliminate cancer cells without damaging host cells. The findings have the potential to develop first-in-class medicines that are designed to be selective for cancer cells and non-toxic to normal cells and tissues. If successful, this discovery may improve the practice of precision medicine by ensuring the right drug is delivered at the right dose at the right time.
Our immune system plays a critical role in our ability to fight off diseases while keeping us healthy. For example, the immune system has the ability to recognize and attack a wide range of infectious pathogens, including bacteria, fungi and protozoa. Researchers at the University of Chicago Medicine Comprehensive Cancer Center were interested in learning whether and how the immune system can mount a similar response against cancer.
Such a discovery could reveal cancer’s weak spot, or Achilles’ heel, and make it possible to develop new, more effective treatments with fewer unwanted side effects.
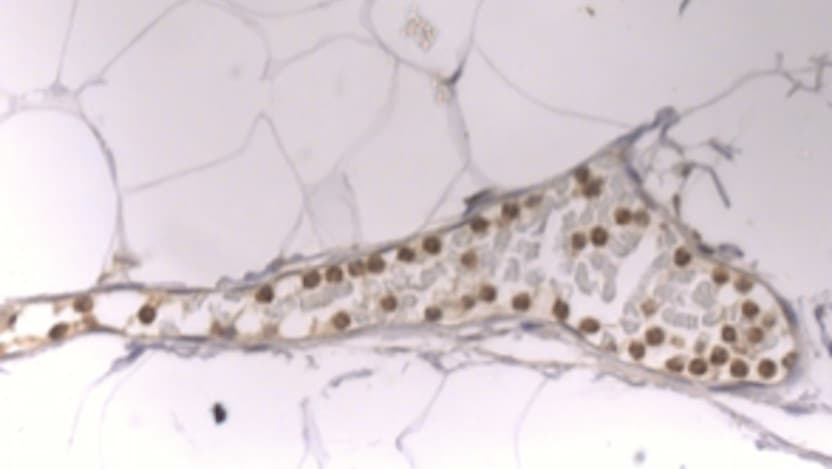
Polymorphonuclear neutrophils (PMNs), a type of white blood cell, provide a strong clue. PMNs respond to chemical signals emitted by the immune system and migrate to different sites in the body where they are needed. However, the exact mechanism by which they cause cancer cells to die is not fully understood.
Through this new study, the team at UChicago identified neutrophil elastase (ELANE) as a major anti-cancer protein released by human neutrophils that activates cell death pathways specifically in cancer cells. ELANE causes cancer cells to die in both tumors and distant locations where they have spread, while sparing nearby healthy cells.
“Taking a step back, what I think we’ve stumbled upon is our body’s first response to mutated cells,” said Lev Becker, PhD, lead author on the paper and associate professor in the Ben May Department for Cancer Research at UChicago. “Cells are constantly changing and mutations accumulate. Some people develop cancer, others do not. The pathway that we’ve discovered may help explain the primordial mechanisms of our immune system to eliminate those mutated cells.”
Using human and mouse models, Becker and colleagues observed that ELANE starts a complex cancer-killing program that suppresses cell survival pathways, induces DNA damage, elevates mitochondrial reactive oxygen species production, and ultimately activates programmed cell death, known as apoptosis.
This chain of events is triggered by PMNs secreting an enzyme called elastase, which breaks down proteins into smaller molecules. As a result, this process liberates the CD95 death domain, a system responsible for keeping the immune system in balance by controlling which cells undergo apoptosis. The activated CD95 death domain then interacts with histone H1, which are elevated in cancer cells to maintain their genomic stability.
ELANE consistently activated this program in many types of cancer cell lines but not in any non-cancer cells tested. According to the researchers, ELANE’s specificity for cancer versus non-cancer cells may limit potential toxicity, a possibility that is strengthened by the lack of side effects observed in tumor-free mice injected with ELANE. This selective killing also preserves immune cells, allowing them to capitalize on liberated antigens and generate a boosted immune response that extends to sites where cancer has spread.
Because it can kill a wide range of cancer cells, the treatment may be able to work whatever the cancer’s genetic make-up. The researchers demonstrated ELANE’s efficacy across nine types of genetically diverse cancer—including difficult-to-treat cancers such as triple-negative breast cancer, melanoma, and lung cancer.
In addition to the discoveries described above, the researchers reported that they uncovered differences between human and mouse neutrophils in releasing active ELANE and showed that porcine pancreatic elastase (PPE), a protein similar to ELANE that is less sensitive to tumor inhibitors, induces an even better therapeutic response.
The researchers said that future studies are warranted to learn how to maximize the therapeutic effects of ELANE/PPE, both as a single therapy and in combination with other cancer treatments.
“This is one of those findings where if we had gone the traditional route of starting in mice we would have never found it,” said Becker. “In this instance, we began with observations from patients, brought it back to the lab to study further in mice, and we are hopeful we’ll be able to bring it back to humans as a novel cancer treatment.”
The unique approach to cancer treatment may be translated to real-world applications. Onchilles Pharma, for which Becker serves as the scientific founder and director, recently received Series A financial backing from investors to advance the first drug candidate based on his work in preclinical proof-of-concept studies.
The study, “Neutrophil elastase selectively kills cancer cells and attenuates tumorigenesis” was funded by the Ludwig Fund for Cancer Research, the Virginia and D.K. Ludwig Fund for Cancer Research, University of Chicago Medicine Comprehensive Cancer Center Janet D. Rowley Discovery Fund, University of Chicago Cancer Research Foundation J. Clifford Moos Award, Ruth Bruch Triple Negative Breast Cancer Research Award, and Women’s Board Faculty Research Startup Funds and Ben May Department Startup Funds.
Additional authors include Chang Cui, Kasturi Chakraborty, Xu Anna Tang, Guolin Zhou, Kelly Q. Schoenfelt, Kristen M. Becker, Alexandria Hoffman, Ya-Fang Chang, Ariane Blank, Catherine A. Reardon, Hilary A. Kenny, Ernst Lengyel, Geoffrey Greene of UChicago; and Tomas Vaisar of the University of Washington, Seattle.
