Could starving ovarian cancer cells of fat block its deadly spread?
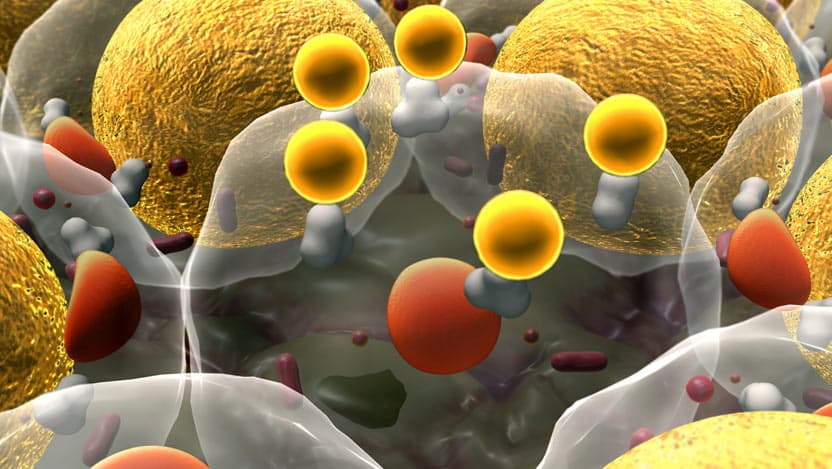
Ovarian cancer can be a devastating disease because it is often not found until it has spread beyond the ovaries to other tissues. It is different from other cancer types because it likes to spread to adipose tissue (body fat), like the abdomen’s fatty area, which provides a rich energy source for these cancer cells. Understanding the biology of ovarian tumors, including why they seem to prefer fatty tissue and how these tumor cells absorb and use fats for energy, is critical to figuring out how to starve these tumor cells and prevent them from spreading.
Physicians-scientists from the University of Chicago Medicine Comprehensive Cancer Center Ernst Lengyel, MD, PhD, Professor and Chair of the Department of Obstetrics and Gynecology, and Iris Romero, MD, Professor of Obstetrics and Gynecology, are unraveling this complex biology to understand ovarian cancer and block its spread.
To understand cancer cells, it’s critical to know how they take in and use energy, or in other words, their metabolism. When cells transform into cancer, their metabolism is reprogrammed to allow the cells to take advantage of their environment and use all available sources of energy to support rapid growth. Investigating the altered metabolism of cancer cells can reveal new ways to attack and starve these cells.
Investigating the altered metabolism of cancer cells can reveal new ways to attack and starve these cells.
In a recent study, Lengyel and Romero reasoned that altered metabolism in cancer cells has similarities to metabolic disorders in individuals. That study tested the idea that drugs already approved to treat metabolic diseases, like diabetes, might be able to regulate cancer cell metabolism to block cancer progression. In 2019, found a specific metabolic target that helps ovarian cancer cells use fats, called fatty acid-binding protein (FABP4). They discovered that ovarian cancer cells that spread to the fatty tissue of the abdomen have high levels of FABP4, and it lets them use the fats to grow and spread.
They followed up their discovery by asking if blocking FABP4 could effectively starve metastatic ovarian cancer cells. In laboratory experiments, they showed that blocking FABP4 slows down ovarian cancer growth. They next tested a FABP4 inhibitor in mice in combination with the standard treatment for ovarian cancer. Their promising results showed that blocking FABP4 reduced the number and size of tumors better than using the standard therapy alone.
The metabolism of fats by ovarian cancer cells not only helps them grow rapidly but also improves their ability to move beyond the abdomen to new sites throughout the body. This occurs because cancer cells that use fats for energy also produce higher levels of unstable metabolic byproducts called reactive oxygen species (ROS). The high levels of ROS can cause further DNA damage to the cancer cells, which allows them to invade new areas in the body.
These investigations of Lengyel, Mukherjee and Romero have provided direction for improved treatment of ovarian cancer. Therapies that block fat metabolism by ovarian cancer cells may prevent these cells from growing in the abdomen and moving to other body sites. Although the treatment used in this study is not approved for use in people, there are other FABP4 inhibitors that are under development and could be investigated for the treatment of ovarian cancer. This clinically relevant work has great potential benefit for ovarian cancer patients in the near future.

Ernst Lengyel, MD, PhD
Ernst Lengyel, MD, PhD, is the Arthur L. and Lee G. Herbst Professor of Obstetrics/Gynecology and chairman of the Department of Obstetrics/Gynecology at UChicago Medicine. He is an internationally known expert in the research and treatment of gynecologic cancers.
View Dr. Lengyel's physician profile
Iris Romero, MD, MS
Iris Romero, MD, MS, is a highly skilled obstetrician and gynecologist with special expertise in cancer prevention. Her clinical practice includes individuals with a family history of gynecologic or breast cancer and patients with genetic mutations that predispose to gynecologic cancers, such as BRCA mutations and others.
View Dr. Romero's physician bio